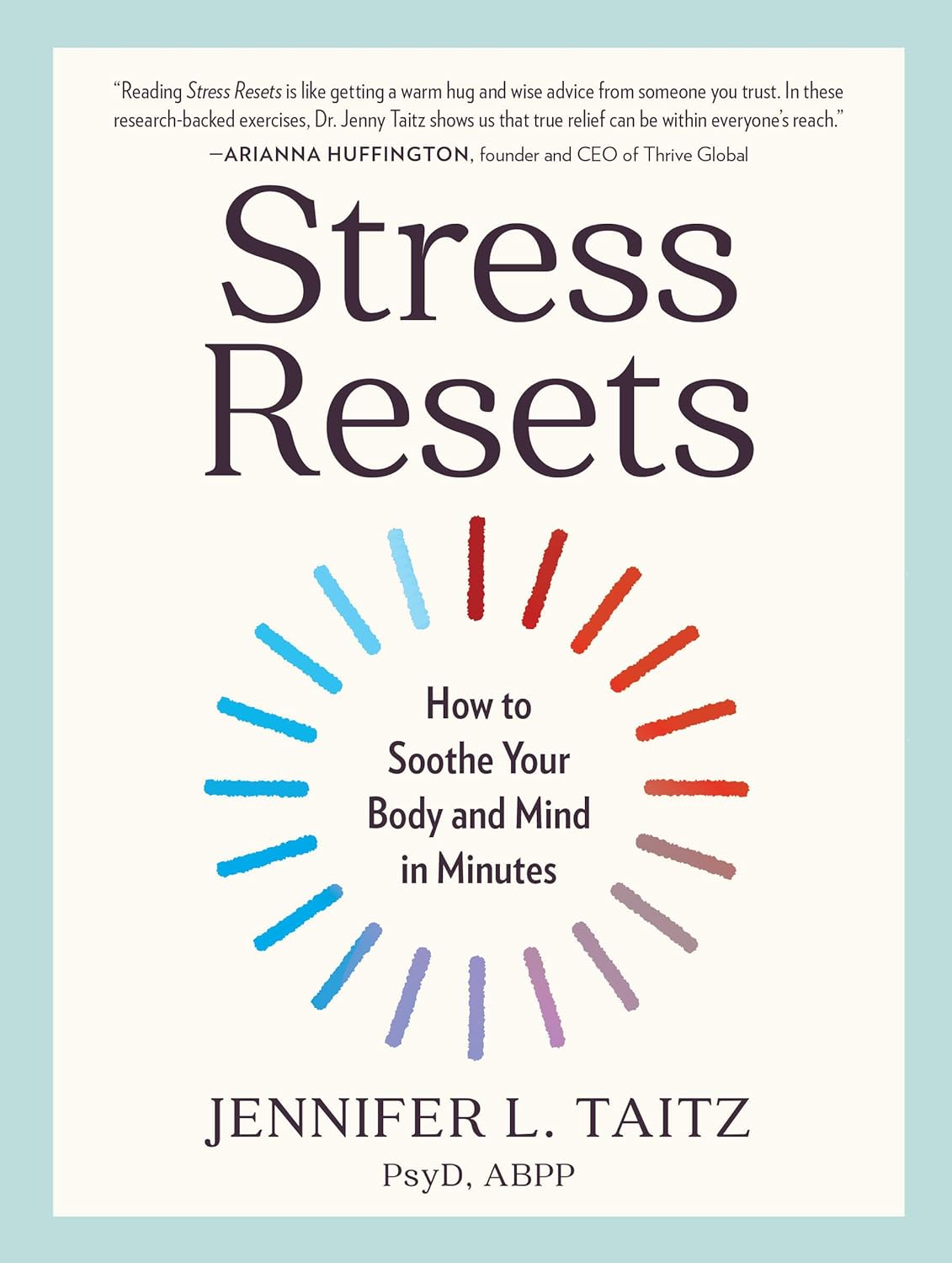
Stress Resets – by Dr. Jennifer Taitz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be thinking: “that’s a bold claim in the subtitle; does the book deliver?”
And yes, yes it does.
The “resets” themselves are divided into categories:
- Mind resets, which are mostly CBT,
- Body resets, which include assorted somatic therapies such as vagus nerve resets, the judicious use of ice-water, what 1-minute sprints of exercise can do for your mental state, and why not to use the wrong somatic therapy for the wrong situation!
- Behavior resets, which are more about the big picture, and not falling into common traps.
What common traps, you ask? This is about how we often have maladaptive responses to stress, e.g. we’re short of money so we overspend, we have an important deadline so we over-research and procrastinate, we’re anxious so we hyperfixate on the problem, we’re grieving so we look to substances to try to cope, we’re exhausted so we stay up late to try to claw back some lost time. Things where our attempt to cope actually makes things worse for us.
Instead, Dr. Taitz advises us of how to get ourselves from “knowing we shouldn’t do that” to actually not doing that, and how to respond more healthily to stress, how to turn general stress into eustress, or as she puts it, how to “turn your knots into bows”.
The style is… “Academic light”, perhaps we could say. It’s a step above pop-science, but a step below pure academic literature, which does make it a very pleasant read as well as informative. There are often footnotes at the bottom of each page to bridge any knowledge-gap, and for those who want to know the evidence of these evidence-based approaches, she does provide 35 pages of hard science sources to back up her claims.
Bottom line: if you’d like to learn how better to manage stress from an evidence-based perspective that’s not just “do minfdulness meditation”, then this book gives a lot of ways.
Click here to check out Stress Resets, and indeed soothe your body and mind in minutes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Vitamin C Worth The Hype? (Doctorly Investigates)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Double Board-Certified Dermatologists Dr. Muneeb Shah & Dr. Luke Maxfield weigh in on vitamin C; is it worth the hype?
Yes it is, but…
There are some caveats, for example:
- It’s best to apply vitamin C on clean, dry skin and let it set before layering other products.
- Avoid mixing with oxidants like benzoyl peroxide (cancels out antioxidant effects).
- Avoid combining with copper (may negate brightening benefits).
- Do not use with hypochlorous acid (oxidative reactions cancel out benefits).
- Be cautious with retinol due to irritation risks.
However, used correctly, it does give very worthy benefits, and they recommend:
- Morning use: acts as an antioxidant, pairs well with sunscreen for better protection from sun and environmental damage.
- Night use: maximizes functions like improving tone, collagen production, texture, and reducing wrinkles.
That’s not to say that at night it stops being an antioxidant or during the day it isn’t critical for collagen synthesis, but it is to say: because of the different things our bodies typically encounter and/or do during the day or night, those are the best times to get the most out of those benefits.
They also review some popular products; here are some notes on their comments about them:
- Skinceuticals C E Ferulic: research-backed, $180, effective but potentially irritating.
- Skinceuticals Phloretin CF: includes 0.5% salicylic acid, good for acne-prone skin.
- Dermatology Vitamin C E Ferulic: relatively more affordable ($70), fragrance-free, includes peptides and ceramides.
- Drunk Elephant C-Firma: powder-to-serum formula, sued for patent infringement.
- Paula’s Choice C15 Booster: reformulated, fragrance-free, similar to Skinceuticals.
- Neutrogena Vitamin C Capsules: stabilized 20% ascorbic acid, single-use, travel-friendly.
- La Roche-Posay Vitamin C Serum: contains fragrance and alcohol, not ideal for sensitive skin.
- Matter of Fact Vitamin C Serum: includes ascorbic acid and ferulic acid, oily texture for dry skin.
- Medik8 Super C Ferulic: stable 30% ethyl ascorbic acid, lightweight texture.
- Naturium Vitamin C Complex: multi-form Vitamin C with niacinamide, alpha arbutin, and turmeric.
- Timeless Vitamin C Serum: affordable ($20), 20% ascorbic acid with E and ferulic acid.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
More Than Skin-Deep: Six Ways To Eat For Healthier Skin ← this one’s about a lot more than just vitamin C 😎
Take care!
Share This Post
-
Why are tall people more likely to get cancer? What we know, don’t know and suspect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People who are taller are at greater risk of developing cancer. The World Cancer Research Fund reports there is strong evidence taller people have a higher chance of of developing cancer of the:
- pancreas
- large bowel
- uterus (endometrium)
- ovary
- prostate
- kidney
- skin (melanoma) and
- breast (pre- and post-menopausal).
But why? Here’s what we know, don’t know and suspect.
Pexels/Andrea Piacquadio Height does increase your cancer risk – but only by a very small amount. Christian Vinces/Shutterstock A well established pattern
The UK Million Women Study found that for 15 of the 17 cancers they investigated, the taller you are the more likely you are to have them.
It found that overall, each ten-centimetre increase in height increased the risk of developing a cancer by about 16%. A similar increase has been found in men.
Let’s put that in perspective. If about 45 in every 10,000 women of average height (about 165 centimetres) develop cancer each year, then about 52 in each 10,000 women who are 175 centimetres tall would get cancer. That’s only an extra seven cancers.
So, it’s actually a pretty small increase in risk.
Another study found 22 of 23 cancers occurred more commonly in taller than in shorter people.
Why?
The relationship between height and cancer risk occurs across ethnicities and income levels, as well as in studies that have looked at genes that predict height.
These results suggest there is a biological reason for the link between cancer and height.
While it is not completely clear why, there are a couple of strong theories.
The first is linked to the fact a taller person will have more cells. For example, a tall person probably has a longer large bowel with more cells and thus more entries in the large bowel cancer lottery than a shorter person.
Scientists think cancer develops through an accumulation of damage to genes that can occur in a cell when it divides to create new cells.
The more times a cell divides, the more likely it is that genetic damage will occur and be passed onto the new cells.
The more damage that accumulates, the more likely it is that a cancer will develop.
A person with more cells in their body will have more cell divisions and thus potentially more chance that a cancer will develop in one of them.
Some research supports the idea having more cells is the reason tall people develop cancer more and may explain to some extent why men are more likely to get cancer than women (because they are, on average, taller than women).
However, it’s not clear height is related to the size of all organs (for example, do taller women have bigger breasts or bigger ovaries?).
One study tried to assess this. It found that while organ mass explained the height-cancer relationship in eight of 15 cancers assessed, there were seven others where organ mass did not explain the relationship with height.
It is worth noting this study was quite limited by the amount of data they had on organ mass.
Is it because tall people have more cells? Halfpoint/Shutterstock Another theory is that there is a common factor that makes people taller as well as increasing their cancer risk.
One possibility is a hormone called insulin-like growth factor 1 (IGF-1). This hormone helps children grow and then continues to have an important role in driving cell growth and cell division in adults.
This is an important function. Our bodies need to produce new cells when old ones are damaged or get old. Think of all the skin cells that come off when you use a good body scrub. Those cells need to be replaced so our skin doesn’t wear out.
However, we can get too much of a good thing. Some studies have found people who have higher IGF-1 levels than average have a higher risk of developing breast or prostate cancer.
But again, this has not been a consistent finding for all cancer types.
It is likely that both explanations (more cells and more IGF-1) play a role.
But more research is needed to really understand why taller people get cancer and whether this information could be used to prevent or even treat cancers.
I’m tall. What should I do?
If you are more LeBron James than Lionel Messi when it comes to height, what can you do?
Firstly, remember height only increases cancer risk by a very small amount.
Secondly, there are many things all of us can do to reduce our cancer risk, and those things have a much, much greater effect on cancer risk than height.
We can take a look at our lifestyle. Try to:
- eat a healthy diet
- exercise regularly
- maintain a healthy weight
- be careful in the sun
- limit alcohol consumption.
And, most importantly, don’t smoke!
If we all did these things we could vastly reduce the amount of cancer.
You can also take part in cancer screening programs that help pick up cancers of the breast, cervix and bowel early so they can be treated successfully.
Finally, take heart! Research also tells us that being taller might just reduce your chance of having a heart attack or stroke.
Susan Jordan, Associate Professor of Epidemiology, The University of Queensland and Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Chocolate & Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chocolate & Health: Fact or Fiction?
“Chocolate Is Good For The Heart”
“When making chocolate chip cookies, you don’t measure using cups, you measure by heart”
…but how good is chocolate when it comes to heart health?
First, what is heart health?
A healthy heart typically has a low resting pulse rate and a strong, steady beat. This is affected strongly by exercise habits, and diet plays only a support role (can’t exercise without energy from food!).
It is also important to have blood pressure within a healthy range (with high blood pressure being a more common problem than low, so things that lower blood pressure are generally considered good).
- Flavanols, flavonoids, and polyphenols in chocolate contribute to lower blood pressure
- Dark chocolate is best for these, as milk chocolate contains much less cocoa solids and more unhelpful fats
- White chocolate contains no cocoa solids and is useless for this
- Some of the fats in most commercial chocolate can contribute to atherosclerosis which raises blood pressure and ultimately can cause heart attacks.
- If you’re diabetic, you will probably not get the usual heart-related benefits from chocolate (sorry)
The Verdict: dark chocolate, in moderation, can support good heart health.
“Chocolate Is Good For The Brain”
Chocolate has been considered a “brain food”… why?
- The brain uses more calories than any other organ (chocolate has many calories)
- The heart benefits we listed above mean improved blood flow—including to your brain
- Chocolate contains phenylethylamine, a powerful chemical that has a similar effect to amphetamines… But it’s metabolized in digestion and never makes it to the central nervous system (so basically, this one’s a miss; we had a good run with the other two, though!)
The Verdict: dark chocolate, in moderation, can support good brain health
“Chocolate Is An Aphrodisiac”
“If chocolate be the food of love, pass me that cocoa; I’m starving”
Most excitingly, chocolate contains phenylethylamine, the “molecule of love” or, more accurately, lust. It has an effect similar to amphetamines, and while we can synthesize it in the body, we can also get it from certain foods. But…
Our body is so keen to get it that most of it is metabolized directly during digestion and doesn’t make it to the brain. Also, chocolate is not as good a source as cabbage—do with that information what you will!
However!
Chocolate contains theobromine and small amounts of caffeine, both stimulants and both generally likely to improve mood; it also contains flavonoids which in turn stimulate production of nitric oxide, which is a relaxant. All in all, things that are convivial to having a good time.
On the other hand…
That relaxation comes specifically with a reduction in blood pressure—something typically considered good for the health for most people most of the time… but that means lowering blood pressure in all parts of your body, which could be the opposite of what you want in intimate moments.
Chocolate also contains zinc, which is essential for hormonal health for most people—the body uses it to produce testosterone and estrogen, respectively. Zinc supplements are popularly sold to those wishing to have more energy in general and good hormonal health in particular, and rightly so. However…
This approach requires long-term supplementation—you can’t just pop a zinc tablet / bar of chocolate / almond before bed and expect immediate results. And if your daily zinc supplementation takes the form of a 3.5oz (100g) bar of chocolate, then you may find it has more effects on your health, and not all of them good!
The Verdict: dark chocolate, in moderation, may promote “the mood”, but could be a double-edged sword when it comes to “the ability”.
“Chocolate Is Good During Menstruation”
The popular wisdom goes that chocolate is rich in iron (of which more is needed during menstruation), and indeed, if you eat 7oz (150g) of dark chocolate made with 85% cocoa, you’ll get a daily a dose of iron (…and nearly 1,000 calories).
More bang-for-buck dietary sources of iron include chickpeas and broccoli, but for some mysterious reason, these are not as commonly reported as popular cravings.
The real explanation for chocolate cravings is more likely that eating chocolate—a food high in sugar and fat along with a chemical bombardment of more specialized “hey, it’s OK, you can relax now” molecules (flavanols/flavonoids, polyphenols, phenylamines, even phenylethylamine, etc) gives a simultaneous dopamine kick (the body’s main “reward” chemical) with a whole-body physiological relaxation… so, little wonder we might crave it in times of stress and discomfort!
The Verdict: it helps, not because it serves a special nutritional purpose, but rather, because the experience of eating chocolate makes us feel good.
Fun fact: Tiramisu (this writer’s favorite dessert) is literally Italian for “pick-me-up”
Share This Post
Related Posts
-
What is PNF stretching, and will it improve my flexibility?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether improving your flexibility was one of your new year’s resolutions, or you’ve been inspired watching certain tennis stars warming up at the Australian Open, maybe 2025 has you keen to focus on regular stretching.
However, a quick Google search might leave you overwhelmed by all the different stretching techniques. There’s static stretching and dynamic stretching, which can be regarded as the main types of stretching.
But there are also some other potentially lesser known types of stretching, such as PNF stretching. So if you’ve come across PNF stretching and it piques your interest, what do you need to know?
Undrey/Shutterstock What is PNF stretching?
PNF stretching stands for proprioceptive neuromuscular facilitation. It was developed in the 1940s in the United States by neurologist Herman Kabat and physical therapists Margaret Knott and Dorothy Voss.
PNF stretching was initially designed to help patients with neurological conditions that affect the movement of muscles, such as polio and multiple sclerosis.
By the 1970s, its popularity had seen PNF stretching expand beyond the clinic and into the sporting arena where it was used by athletes and fitness enthusiasts during their warm-up and to improve their flexibility.
Although the specifics have evolved over time, PNF essentially combines static stretching (where a muscle is held in a lengthened position for a short period of time) with isometric muscle contractions (where the muscle produces force without changing length).
PNF stretching is typically performed with the help of a partner.
There are 2 main types
The two most common types of PNF stretching are the “contract-relax” and “contract-relax-agonist-contract” methods.
The contract-relax method involves putting a muscle into a stretched position, followed immediately by an isometric contraction of the same muscle. When the person stops contracting, the muscle is then moved into a deeper stretch before the process is repeated.
For example, to improve your hamstring flexibility, you could lie down and get a partner to lift your leg up just to the point where you begin to feel a stretch in the back of your thigh.
Once this sensation eases, attempt to push your leg back towards the ground as your partner resists the movement. After this, your partner should now be able to lift your leg up slightly higher than before until you feel the same stretching sensation.
This technique was based on the premise that the contracted muscle would fall “electrically silent” following the isometric contraction and therefore not offer its usual level of resistance to further stretching (called “autogenic inhibition”). The contract-relax method attempts to exploit this brief window to create a deeper stretch than would otherwise be possible without the prior muscle contraction.
The contract-relax-agonist-contract method is similar. But after the isometric contraction of the stretched muscle, you perform an additional contraction of the muscle group opposing the muscle being stretched (referred to as the “agonist” muscle), before the muscle is moved into a static stretch once more.
Again, if you’re trying to improve hamstring flexibility, immediately after trying to push your leg towards the ground you would attempt to lift it back towards the ceiling (this bit without partner resistance). You would do this by contracting the muscles on the front of the thigh (the quadriceps, the agonist muscle in this case).
Likewise, after this, your partner should be able to lift your leg up slightly higher than before.
The contract-relax-agonist-contract method is said to take advantage of a phenomenon known as “reciprocal inhibition.” This is where contracting the muscle group opposite that of the muscle being stretched leads to a short period of reduced activation of the stretched muscle, allowing the muscle to stretch further than normal.
What does the evidence say?
Research has shown PNF stretching is associated with improved flexibility.
While it has been suggested that both PNF methods improve flexibility via changes in nervous system function, research suggests they may simply improve our ability to tolerate stretching.
It’s worth noting most of the research on PNF stretching and flexibility has focused on healthy populations. This makes it difficult to provide evidence-based recommendations for people with clinical conditions.
And it may not be the most effective method if you’re looking to improve your flexibility in the long term. A 2018 review found static stretching was better for improving flexibility compared to PNF stretching. But other research has found it could offer greater immediate benefits for flexibility than static stretching.
At present, similar to other types of stretching, research linking PNF stretching to injury prevention and improved athletic performance is relatively inconclusive.
PNF stretching may actually lead to small temporary deficits in performance of strength, power, and speed-based activities if performed immediately beforehand. So it’s probably best done after exercise or as a part of a standalone flexibility session.
Static stretching may be a more effective way to improve flexibility over the long-term. GaudiLab/Shutterstock How much should you do?
It appears that a single contract-relax or contract-relax-agonist-contract repetition per muscle, performed twice per week, is enough to improve flexibility.
The contraction itself doesn’t need to be hard and forceful – only about 20% of your maximal effort should suffice. The contraction should be held for at least three seconds, while the static stretching component should be maintained until the stretching sensation eases.
So PNF stretching is potentially a more time-efficient way to improve flexibility, compared to, for example, static stretching. In a recent study we found four minutes of static stretching per muscle during a single session is optimal for an immediate improvement in flexibility.
Is PNF stretching the right choice for me?
Providing you have a partner who can help you, PNF stretching could be a good option. It might also provide a faster way to become more flexible for those who are time poor.
However, if you’re about to perform any activities that require strength, power, or speed, it may be wise to limit PNF stretching to afterwards to avoid any potential deficits in performance.
Lewis Ingram, Lecturer in Physiotherapy, University of South Australia and Hunter Bennett, Lecturer in Exercise Science, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What to Know About Stillbirths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Series: Stillbirths:When Babies Die Before Taking Their First Breath
The U.S. has not prioritized stillbirth prevention, and American parents are losing babies even as other countries make larger strides to reduce deaths late in pregnancy.
Every year, more than 20,000 pregnancies in the U.S. end in a stillbirth, the death of an expected child at 20 weeks or more of pregnancy. Research shows as many as 1 in 4 stillbirths may be preventable. We interviewed dozens of parents of stillborn children who said their health care providers did not tell them about risk factors or explain what to watch for while pregnant. They said they felt blindsided by what followed. They did not have the information needed to make critical decisions about what happened with their baby’s body, about what additional testing could have been done to help determine what caused the stillbirth, or about how to navigate the process of requesting important stillbirth documents.
This guide is meant to help fill the void of information on stillbirths. It’s based on more than 150 conversations with parents, health care providers, researchers and other medical experts.
Whether you’re trying to better prepare for a pregnancy or grieving a loss, we hope this will help you and your family. This guide does not provide medical advice. We encourage you to seek out other reliable resources and consult with providers you trust.
We welcome your thoughts and questions at mailto:[email protected]. You can share your experience with stillbirth with us. If you are a health care provider interested in distributing this guide, let us know if we can help.
Table of contents:
- What Is Stillbirth?
- Are Stillbirths Preventable?
- What to Expect After a Stillbirth.
- Grieving After a Stillbirth.
- What You Might Say and Do After a Loved One Experiences a Stillbirth.
What Is Stillbirth?
Many people told us that the first time they heard the term stillbirth was after they delivered their stillborn baby. In many cases, the lack of information and awareness beforehand contributed to their heartache and guilt afterward.
Stillbirth is defined in the U.S. as the death of a baby in the womb at 20 weeks or more of pregnancy. Depending on when it happens, stillbirth is considered:
- Early: 20-27 weeks of pregnancy.
- Late: 28-36 weeks of pregnancy.
- Term: 37 or more weeks of pregnancy.
About half of all stillbirths in the U.S. occur at 28 weeks or later.
What is the difference between a stillbirth and a miscarriage?
Both terms describe pregnancy loss. The distinction is when the loss occurs. A miscarriage is typically defined as a loss before the 20th week of pregnancy, while stillbirth is after that point.
How common is stillbirth?
Each year, about 1 in 175 deliveries in the U.S. are stillbirths — that’s about 60 stillborn babies every day — making it one of the most common adverse pregnancy outcomes, but it is rarely discussed.
If you are surprised by that fact, you are not alone. Many people we spoke to did not know how common stillbirths are. Leandria Lee of Texas said she spent her 2021 pregnancy unaware that her daughter, Zuri Armoni, could die in the last phase of her pregnancy.
“If I was prepared to know that something could happen, I don’t think it would have been as bad. But to not know and then it happens, it affects you,” she said of her stillbirth at 35 weeks.
Some doctors have told us they don’t introduce the possibility of a stillbirth because they don’t want to create additional anxiety for patients.
Other doctors say withholding information leaves patients unprepared.
“We have this idea that we can’t scare the patient, which to me is very paternalistic,” said Dr. Heather Florescue, an OB-GYN near Rochester, New York, who works to inform doctors and patients about stillbirth prevention.
What causes stillbirths?
There is a lot we don’t know about stillbirths because there hasn’t been enough research. The cause of the stillbirth is unknown in about 1 in 3 cases.
What we do know is that a number of factors may cause or increase the risk of a stillbirth, including:
- The baby not growing as expected.
- Placental abnormalities or problems with the umbilical cord.
- Genetic or structural disorders that cause developmental issues.
- High blood pressure before pregnancy or preeclampsia, a potentially fatal complication that usually appears late in pregnancy and causes high blood pressure.
- Diabetes before or during pregnancy.
- An infection in the fetus, the placenta or the pregnant person.
- Smoking.
- Being 35 or older.
- Obesity.
- Being pregnant with more than one baby.
But not all doctors, hospitals or health departments perform tests to identify the potential cause of a stillbirth or determine if it could have been prevented. Even when a cause is identified, fetal death records are rarely updated. This means data is sometimes inaccurate. Researchers strongly encourage doctors to perform a stillbirth evaluation, which includes an examination of the placenta and umbilical cord, a fetal autopsy and genetic testing.
If your hospital or doctor does not proactively offer one or more of these exams, you can ask them to conduct the tests. Research shows that placental exams may help establish a cause of death or exclude a suspected one in about 65% of stillbirths, while autopsies were similarly useful in more than 40% of cases.
Are Stillbirths Preventable?
Not all stillbirths are preventable, but some are. For pregnancies that last 37 weeks or more, one study found that nearly half of stillbirths are potentially preventable.
Dr. Joanne Stone, who last year was president of the Society of Maternal-Fetal Medicine, leads the country’s first Rainbow Clinic at Mount Sinai Hospital in New York. The clinic is modeled on similar facilities in the United Kingdom that care for people who want to conceive again after a stillbirth. She said many doctors used to think there was nothing they could do to prevent stillbirth.
“People just looked at it like, ‘Oh, it was an accident, couldn’t have been prevented,’” said Stone, who also is the system chair of the obstetrics, gynecology and reproductive science department at the Icahn School of Medicine. “But we know now there are things that we can do to try to prevent that from happening.”
She said doctors can:
- More closely monitor patients with certain risk factors, like high blood pressure, diabetes or obesity.
- Ask about prior infant loss or other obstetrical trauma.
- Carefully assess whether a baby’s growth is normal.
- Work to diagnose genetic anomalies.
- Teach patients how to track their baby’s movements and encourage them to speak up if they notice activity has slowed or stopped.
- Deliver at or before 39 weeks if there are concerns.
What are the risks of stillbirth over the course of a pregnancy?
The risk of a stillbirth increases significantly toward the end of pregnancy, especially after 39 weeks. The risk is higher for people who get pregnant at 35 or older. The risk begins to climb even earlier, around 36 weeks, for people pregnant with twins.
What you and your doctor can do to reduce the risk of stillbirth.
While federal agencies in the U.S. have yet to come up with a checklist that may help reduce the risk of stillbirth, the Stillbirth Centre of Research Excellence in Australia has adopted a Safer Baby Bundle that lists five recommendations:
- Stop smoking.
- Regularly monitor growth to reduce the risk of fetal growth restriction, when the fetus is not growing as expected.
- Understand the importance of acting quickly if fetal movement decreases.
- Sleep on your side after 28 weeks.
- Talk to your doctor about when to deliver. Depending on your situation, it may be before your due date.
The American College of Obstetricians and Gynecologists has compiled a list of tests and techniques doctors can use to try to reduce the risk of a stillbirth. They include:
- A risk assessment to identify prenatal needs.
- A nonstresstest, which checks the fetus’s heart rate and how it changes as the fetus moves.
- A biophysical profile, which is done with an ultrasound to measure body movement, muscle tone and breathing, along with amniotic fluid volume.
The group stressed that there is no test that can guarantee a stillbirth won’t happen and that individual circumstances should determine what tests are run.
Are some people at higher risk for stillbirth?
Black women are more than twice as likely to have a stillbirth as white women. There are a number of possible explanations for that disparity, including institutional bias and structural racism, and a patient’s pre-pregnancy health, socioeconomic status and access to health care. In addition, research shows that Black women are more likely than white women to experience multiple stressful life events while pregnant and have their concerns ignored by their health care provider. Similar racial disparities drive the country’s high rate of maternal mortality.
How to find a provider you trust.
Finding a doctor to care for you during your pregnancy can be a daunting process. Medical experts and parents suggest interviewing prospective providers before you decide on the right one.
Here is a short list of questions you might want to ask a potential OB-GYN:
- What is the best way to contact you if I have questions or concerns?
- How do you manage inquiries after hours and on weekends? Do you see walk-ins?
- How do you manage prenatal risk assessments?
- What should I know about the risks of a miscarriage or stillbirth?
- How do you decide when a patient should be induced?
If a provider doesn’t answer your questions to your satisfaction, don’t be reluctant to move on. Dr. Ashanda Saint Jean, chair of the obstetrics and gynecology department at HealthAlliance Hospitals of the Hudson Valley in New York, said she encourages her patients to find the provider that meets their needs.
“Seek out someone that is like-minded,” said Saint Jean “It doesn’t have to be that they’re the same ethnicity or the same race, but like-minded in terms of the goals of what that patient desires for their own health and prosperity.”
What to know in the last trimester.
The last trimester can be an uncomfortable and challenging time as the fetus grows and you get increasingly tired. During this critical time, your provider should talk to you about the following topics:
- Whether you need a nonstress test to determine if the fetus is getting enough oxygen.
- The best way to track fetal movements.
- What to do if your baby stops moving.
- Whether you are at risk for preeclampsia or gestational diabetes.
Rachel Foran’s child, Eoin Francis, was stillborn at 41 weeks and two days. Foran, who lives in New York, said she believes that if her doctor had tracked her placenta, and if she had understood the importance of fetal movement, she and her husband might have decided to deliver sooner.
She remembers that her son was “very active” until the day before he was stillborn.
“I would have gone in earlier if someone had told me, ‘You’re doing this because the baby could die,’” she said of tracking fetal movement. “That would have been really helpful to know.”
Researchers are looking at the best way to measure the health, blood flow and size of the placenta, but studies are still in their early stages.
“If someone had been doing that with my son’s,” Foran said, “my son would be alive.”
A placental exam and an autopsy showed that a small placenta contributed to Foran’s stillbirth.
How often should you feel movement?
Every baby and each pregnancy are different, so it is important to get to know what levels of activity are normal for you. You might feel movement around 20 weeks. You’re more likely to feel movement when you’re sitting or lying down. Paying attention to movement during the third trimester is particularly important because research shows that changes, including decreased movement or bursts of excessive activity, are associated with an increased risk of stillbirth. Most of the time, it’s nothing. But sometimes it can be a sign that your baby is in distress. If you’re worried, don’t rely on a home fetal doppler to reassure you. Reach out to your doctor.
Saint Jean offers a tip to track movement: “I still tell patients each day to lay on their left side after dinner and record how many times their baby moves, because then that will give you an idea of what’s normal for your baby,” she said.
Other groups recommend using the Count the Kicks app as a way of tracking fetal movements and establishing what is normal for that pregnancy. Although there is no scientific consensus that counting kicks can prevent stillbirths, the American College of Obstetricians and Gynecologists and other groups recommend that patients be aware of fetal movement patterns.
Dr. Karen Gibbins is a maternal-fetal medicine specialist at Oregon Health & Science University who in 2018 had stillborn son named Sebastian. She said the idea that babies don’t move as much at the end of pregnancy is a dangerous myth.
“You might hear that babies slow down at the end,” she said. “They don’t slow down. They just have a little less space. So their movements are a little different, but they should be as strong and as frequent.”
What to Expect After a Stillbirth
What might happen at the hospital?
Parents are often asked to make several important decisions while they are still reeling from the shock and devastation of their loss. It’s completely understandable if you need to take some time to consider them.
Some other things you can ask for (if medical personnel don’t offer them) are:
- Blood work, a placental exam, an autopsy and genetic testing.
- A social worker or counselor, bereavement resources and religious or chaplain support.
- The option to be isolated from the labor rooms.
- Someone to take photos of you and your baby, typically either a nurse or an outside group.
- A small cooling cot that allows parents to spend more time with their babies after a stillbirth. If one is not available, you can ask for ice packs to put in the swaddle or the bassinet.
- A mold of your baby’s hands and feet.
- Information about burial or cremation services.
- Guidance on what to do if your milk comes in.
Getting an autopsy after a stillbirth.
Whether to have an autopsy is a personal decision. It may not reveal a cause of death, but it might provide important information about your stillbirth and contribute to broader stillbirth research. Autopsies can be useful if you are considering another pregnancy in the future. Families also told us that an autopsy can help parents feel they did everything they could to try to understand why their baby died.
But several families told us their health care providers didn’t provide them with the right information to help with that decision. Some aren’t trained in the advantages of conducting an autopsy after a stillbirth, or in when and how to sensitively communicate with parents about it. Some, for example, don’t explain that patients can still have an open-casket funeral or other service after an autopsy because the incisions can easily be covered by clothing. Others may not encourage an autopsy because they think they already know what caused the stillbirth or don’t believe anything could have been done to prevent it. In addition, not all hospitals have the capacity to do an autopsy, but there may be private autopsy providers that can perform one at an additional cost.
You can read more about autopsies in our reporting.
Paying for an autopsy after a stillbirth.
If you decide you want an autopsy, you may wonder whether you need to pay out-of-pocket for it. Several families told us their providers gave them incomplete or incorrect information. Many larger or academic hospitals offer autopsies at no cost to patients. Some insurance companies also cover the cost of an autopsy after a stillbirth.
When hospitals don’t provide an autopsy, they may give you names of private providers. That was the case for Rachel Foran. The hospital gave her and her husband a list of numbers to call if they wanted to pay for an autopsy themselves. The process, she said, shocked her.
“I had just delivered and we had to figure out what to do with his body,” Foran said. “It felt totally insane that that was what we had to do and that we had to figure it out on our own.”
An independent autopsy, records show, cost them $5,000.
What is a certificate of stillbirth and how do I get one?
A fetal death certificate is the official legal document that records the death. This is the document used to gather data on and track the number of stillbirths in the country. Many states also issue a certificate of stillbirth or a certificate of birth resulting in stillbirth, which acknowledge the baby’s birth. Families told us they appreciated having that document, since typical birth certificates are not issued for stillbirths. You can usually request a certificate from the vital records office.
Grieving After a Stillbirth
What are the effects of stillbirths on parents and families?
Over and over, families told us the effects of losing a baby can reverberate for a lifetime.
Bereavement support groups may help provide a space to share experiences and resources. Hospitals and birth centers may suggest a local grief group.
We talked with Anna Calix, a maternal health expert who became active in perinatal loss prevention after her son Liam was stillborn on his due date in 2016. Calix leads grief support groups for people of color in English and Spanish.
She suggested rededicating the time you would have spent taking care of a new baby to the grief process.
“You can do that by addressing your own thoughts and feelings and really experiencing those feelings,” Calix said. “We like to push those feelings away or try to do something to distract and avoid, but no matter what we do, the feelings are there.”
It’s important, she said, to give yourself permission to grow your connection with your child and work through thoughts of guilt or blame.
What You Might Say and Do After a Loved One Experiences a Stillbirth
Finding the right words can be difficult. The following are a few suggestions from parents who went through a stillbirth.
Helpful:
- Acknowledge the loss and offer condolences.
- Ask if the baby was named and use the name.
- Allow space for the family to talk about their baby.
Unhelpful:
- Avoid talking about the baby.
- Minimize the loss or compare experiences.
- Start statements with “at least.”
Suggested phrases to avoid:
- “You’re young. You can have more kids.”
- “At least you have other children.”
- “These things just happen.”
- “Your baby is in a better place now.”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between autism and Asperger’s disorder?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Swedish climate activist Greta Thunberg describes herself as having Asperger’s while others on the autism spectrum, such as Australian comedian Hannah Gatsby, describe themselves as “autistic”. But what’s the difference?
Today, the previous diagnoses of “Asperger’s disorder” and “autistic disorder” both fall within the diagnosis of autism spectrum disorder, or ASD.
Autism describes a “neurotype” – a person’s thinking and information-processing style. Autism is one of the forms of diversity in human thinking, which comes with strengths and challenges.
When these challenges become overwhelming and impact how a person learns, plays, works or socialises, a diagnosis of autism spectrum disorder is made.
Where do the definitions come from?
The Diagnostic and Statistical Manual of Mental Disorders (DSM) outlines the criteria clinicians use to diagnose mental illnesses and behavioural disorders.
Between 1994 and 2013, autistic disorder and Asperger’s disorder were the two primary diagnoses related to autism in the fourth edition of the manual, the DSM-4.
In 2013, the DSM-5 collapsed both diagnoses into one autism spectrum disorder.
How did we used to think about autism?
The two thinkers behind the DSM-4 diagnostic categories were Baltimore psychiatrist Leo Kanner and Viennese paediatrician Hans Asperger. They described the challenges faced by people who were later diagnosed with autistic disorder and Asperger’s disorder.
Kanner and Asperger observed patterns of behaviour that differed to typical thinkers in the domains of communication, social interaction and flexibility of behaviour and thinking. The variance was associated with challenges in adaptation and distress.
Kanner and Asperger described different thinking patterns in children with autism.
Roman Nerud/ShutterstockBetween the 1940s and 1994, the majority of those diagnosed with autism also had an intellectual disability. Clinicians became focused on the accompanying intellectual disability as a necessary part of autism.
The introduction of Asperger’s disorder shifted this focus and acknowledged the diversity in autism. In the DSM-4 it superficially looked like autistic disorder and Asperger’s disorder were different things, with the Asperger’s criteria stating there could be no intellectual disability or delay in the development of speech.
Today, as a legacy of the recognition of the autism itself, the majority of people diagnosed with autism spectrum disorder – the new term from the DSM-5 – don’t a have an accompanying intellectual disability.
What changed with ‘autism spectrum disorder’?
The move to autism spectrum disorder brought the previously diagnosed autistic disorder and Asperger’s disorder under the one new diagnostic umbrella term.
It made clear that other diagnostic groups – such as intellectual disability – can co-exist with autism, but are separate things.
The other major change was acknowledging communication and social skills are intimately linked and not separable. Rather than separating “impaired communication” and “impaired social skills”, the diagnostic criteria changed to “impaired social communication”.
The introduction of the spectrum in the diagnostic term further clarified that people have varied capabilities in the flexibility of their thinking, behaviour and social communication – and this can change in response to the context the person is in.
Why do some people prefer the old terminology?
Some people feel the clinical label of Asperger’s allowed a much more refined understanding of autism. This included recognising the achievements and great societal contributions of people with known or presumed autism.
The contraction “Aspie” played an enormous part in the shift to positive identity formation. In the time up to the release of the DSM-5, Tony Attwood and Carol Gray, two well known thinkers in the area of autism, highlighted the strengths associated with “being Aspie” as something to be proud of. But they also raised awareness of the challenges.
What about identity-based language?
A more recent shift in language has been the reclamation of what was once viewed as a slur – “autistic”. This was a shift from person-first language to identity-based language, from “person with autism spectrum disorder” to “autistic”.
The neurodiversity rights movement describes its aim to push back against a breach of human rights resulting from the wish to cure, or fundamentally change, people with autism.
Autism is one of the forms of diversity in human thinking, which comes with strengths and challenges.
Alex and Maria photo/ShutterstockThe movement uses a “social model of disability”. This views disability as arising from societies’ response to individuals and the failure to adjust to enable full participation. The inherent challenges in autism are seen as only a problem if not accommodated through reasonable adjustments.
However the social model contrasts itself against a very outdated medical or clinical model.
Current clinical thinking and practice focuses on targeted supports to reduce distress, promote thriving and enable optimum individual participation in school, work, community and social activities. It doesn’t aim to cure or fundamentally change people with autism.
A diagnosis of autism spectrum disorder signals there are challenges beyond what will be solved by adjustments alone; individual supports are also needed. So it’s important to combine the best of the social model and contemporary clinical model.
Andrew Cashin, Professor of Nursing, School of Health and Human Sciences, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: