Parsnips vs Potatoes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing parsnips to potatoes, we picked the parsnips.
Why?
To be more specific, we’re looking at russet potatoes, and in both cases we’re looking at cooked without fat or salt, skin on. In other words, the basic nutritional values of these plants in edible form, without adding anything. With this in mind, once we get to the root of things, there’s a clear winner:
Looking at the macros first, potatoes have more carbs while parsnips have more fiber. Potatoes do have more protein too, but given the small numbers involved when it comes to protein we don’t think this is enough of a plus to outweigh the extra fiber in the parsnips.
In the category of vitamins, again a champion emerges: parsnips have more of vitamins B1, B2, B5, B9, C, E, and K, while potatoes have more of vitamins B3, B6, and choline. So, a 7:3 win for parsnips.
When it comes to minerals, parsnips have more calcium copper, manganese, selenium, and zinc, while potatoes have more iron and potassium. Potatoes do also have more sodium, but for most people most of the time, this is not a plus, healthwise. Disregarding the sodium, this category sees a 5:2 win for parsnips.
In short: as with most starchy vegetables, enjoy both in moderation if you feel so inclined, but if you’re picking one, then parsnips are the nutritionally best choice here.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Should You Go Light Or Heavy On Carbs?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Compact Tai Chi – by Dr. Jesse Tsao
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A very frustrating thing when practicing tai chi, especially when learning, is the space typically required. We take a step this way and lunge that way and turn and now we’ve kicked a bookcase. Add a sword, and it’s goodnight to the light fixtures at the very least.
While a popular suggestion may be “do it outside”, we do not all have the luxury of living in a suitable climate. We also may prefer to practice in private, with no pressing urge to have an audience.
Tsao’s book, therefore, is very welcome. But how does he do it? The very notion of constriction is antithetical to tai chi, after all.
He takes the traditional forms, keeps the movements mostly the same, and simply changes the order of them. This way, the practitioner revolves around a central point. Occasionally, a movement will become a smaller circle than it was, but never in any way that would constrict movement.
Of course, an obvious question for any such book is “can one learn this from a book?” and the answer is complex, but we would lean towards yes, and insofar as one can learn any physical art from a book, this one does a fine job. It helps that it builds up progressively, too.
All in all, this book is a great choice for anyone who’s interested in taking up tai chi, and/but would like to do so without leaving their home.
Share This Post
-
Stress Resets – by Dr. Jennifer Taitz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be thinking: “that’s a bold claim in the subtitle; does the book deliver?”
And yes, yes it does.
The “resets” themselves are divided into categories:
- Mind resets, which are mostly CBT,
- Body resets, which include assorted somatic therapies such as vagus nerve resets, the judicious use of ice-water, what 1-minute sprints of exercise can do for your mental state, and why not to use the wrong somatic therapy for the wrong situation!
- Behavior resets, which are more about the big picture, and not falling into common traps.
What common traps, you ask? This is about how we often have maladaptive responses to stress, e.g. we’re short of money so we overspend, we have an important deadline so we over-research and procrastinate, we’re anxious so we hyperfixate on the problem, we’re grieving so we look to substances to try to cope, we’re exhausted so we stay up late to try to claw back some lost time. Things where our attempt to cope actually makes things worse for us.
Instead, Dr. Taitz advises us of how to get ourselves from “knowing we shouldn’t do that” to actually not doing that, and how to respond more healthily to stress, how to turn general stress into eustress, or as she puts it, how to “turn your knots into bows”.
The style is… “Academic light”, perhaps we could say. It’s a step above pop-science, but a step below pure academic literature, which does make it a very pleasant read as well as informative. There are often footnotes at the bottom of each page to bridge any knowledge-gap, and for those who want to know the evidence of these evidence-based approaches, she does provide 35 pages of hard science sources to back up her claims.
Bottom line: if you’d like to learn how better to manage stress from an evidence-based perspective that’s not just “do minfdulness meditation”, then this book gives a lot of ways.
Click here to check out Stress Resets, and indeed soothe your body and mind in minutes!
Share This Post
-
Aging Solo – by Ellen Dawson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us will face the challenge of “aging solo”, if indeed we’re not already. The premise of this book is that while it may indeed be a challenge, it can be an exciting challenge rather than a scary one.
Thus, Dawson bids us empower ourselves to tackle it head on, proactively.
To that end, she offers her “EMPOWER” framework:
- Embrace the challenge of living solo
- Manage money mindfully while welcoming desires
- Prioritize vitality and live a vibrant life
- Own your identity; build resilience and confidence
- Weave bonds: build and maintain relationships (solo doesn’t mean lacking connections!
- Energize yourself and discover new passions
- Renew yourself and create a joyful environment
Now, as listed, those may seem a little vague, but rest assured she goes into great detail in the book, with a whole chapter for each.
For example, prioritizing vitality and energizing oneself can seem like a double-up, but the former chapter is about healthy living in the context of the solo life, while the latter chapter is more about avocation lifelong learning, overcoming fear of the unknown, and making sure to actually live this one precious life, not just go through the motions.
The style is energetic and motivational, and yet backed up with 19 pages of scientific references.
Bottom line: this book is, in essence, a roadmap for aging solo and creating the future we deserve, on our own terms. An enjoyable, practical, and uplifting read!
Click here to check out Aging Solo, and thrive as a “Soloist”!
Share This Post
Related Posts
-
Fennel vs Artichoke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fennel to artichoke, we picked the artichoke.
Why?
Both are great! But artichoke wins on nutritional density.
In terms of macros, artichoke has more protein and more fiber, for only slightly more carbs.
Vitamins are another win for artichoke, boasting more of vitamins B1, B2, B3, B5, B6, B9, and choline. Meanwhile, fennel has more of vitamins A, E, and K, which is also very respectable but does allow artichoke a 6:3 lead.
In the category of minerals, artichoke has a lot more copper, iron, magnesium, manganese, and phosphorus, while fennel has a little more calcium, potassium, and selenium.
One other relevant factor is that fennel is a moderate appetite suppressant, which may be good or bad depending on your food-related goals.
All in all though, we say the artichoke wins by virtue of its greater abundance of nutrients!
Want to learn more?
You might like to read:
What Matters Most For Your Heart? ← appropriately enough, with fennel hearts and artichoke hearts!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chetna’s Healthy Indian – by Chetna Makan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Indian food is wonderful—a subjective opinion perhaps, but a popular view, and one this reviewer certainly shares. And of course, cooking with plenty of vegetables and spices is a great way to get a lot of health benefits.
There are usually downsides though, such as that in a lot of Indian cookbooks, every second thing is deep-fried, and what’s not deep-fried contains an entire day or more’s saturated fat content in ghee, and a lot of sides have more than their fair share of sugar.
This book fixes all that, by offering 80 recipes that prioritize health without sacrificing flavor.
The recipes are, as the title suggests, vegetarian, though many are not vegan (yogurt and cheese featuring in many recipes). That said, even if you are vegan, it’s pretty easy to veganize those with the obvious plant-based substitutions. If you have soy yogurt and can whip up vegan paneer yourself (here’s our own recipe for that), you’re pretty much sorted.
The cookbook strikes a good balance of being neither complicated nor “did we really need a recipe for this?” basic, and delivers value in all of its recipes. The ingredients, often a worry for many Westerners, should be easily found if you have a well-stocked supermarket near you; there’s nothing obscure here.
Bottom line: if you’d like to cook more Indian food and want your food to be exciting without also making your blood pressure exciting, then this is an excellent book for keeping you well-nourished, body and soul.
Click here to check out Chetna’s Healthy Indian, and spice up your culinary repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
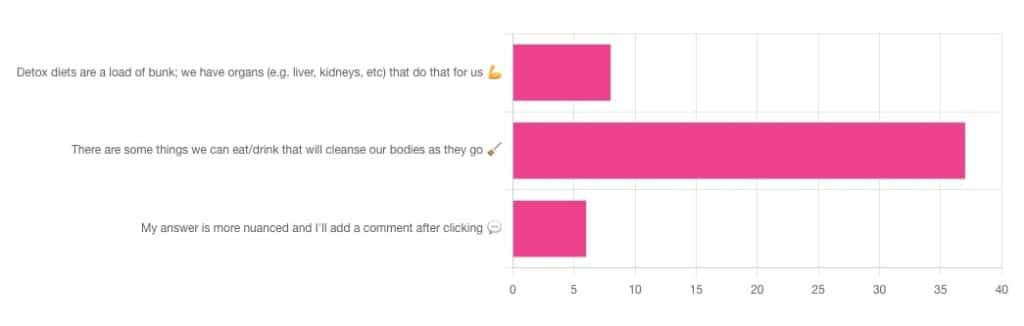
Out of the subscribers who engaged in the poll, it looks like we have a lot of confidence in at least some detox approaches being useful!
Celery juice is most people’s go-to, and indeed it was the only one to get mentioned in the comments added. So let’s take a look at that first…
Celery juice
Celery juice is enjoyed by many people, with many health benefits in mind, including to:
- reduce inflammation
- lower blood pressure
- heal the liver
- fight cancer
- reduce bloating
- support the digestive system
- increase energy
- support weight loss
- promote good mental health
An impressive list! With such an impressive list, we would hope for an impressive weight of evidence, so regular readers might be wondering why those bullet-pointed items aren’t all shiny hyperlinks to studies backing those claims. The reason is…
There aren’t any high-quality studies that back any of those claims.
We found one case study (so, a study with a sample size of one; not amazing) that observed a blood pressure change in an elderly man after drinking celery juice.
Rather than trawl up half of PubMed to show the lacklustre results in a way more befitting of Research Review Monday, though, here’s a nice compact article detailing the litany of disappointment that is science’s observations regards celery juice:
Why Are People Juicing Their Celery? – by Allison Webster, PhD, RD
A key take-away is: juicing destroys the fiber that is celery’s biggest benefit, and its phytochemicals are largely unproven to be of use.
If you enjoy celery, great! It (when not juiced) is a great source of fiber and water. If you juice it, it’s a great source of water.
Activated Charcoal
Unlike a lot of greenery—whose “cleansing” benefits mostly come from fiber and disappear when juiced—activated charcoal has a very different way of operating.
Activated charcoal is negatively charged on a molecular level*, and that—along with its porous nature—traps toxins. It really is a superpowered detox that actually works very well indeed.
But…
It works very well indeed. It will draw out toxins so well, that it’s commonly used to treat poisonings. “Wait”, we hear you say, “why was that a but”?
It doesn’t know what a toxin is. It just draws out all of the things. You took medicine recently? Not any more you didn’t. You didn’t even take that medication orally, you took it some other way? Activated charcoal does not care:
- The effect of activated charcoal on drug exposure following intravenous administration: A meta-analysis
- Activated charcoal for acute overdose: a reappraisal
Does this mean that activated charcoal can be used to “undo” a night of heavy drinking?
Sadly not. That’s one of the few things it just doesn’t work for. It won’t work for alcohol, salts, or metals:
The Use of Activated Charcoal to Treat Intoxications
*Fun chemistry mnemonic about ions:
Cations are pussitive
Anions (by process of elimination) are negative
Onions taste good in salad (remember also: Cole’s Law)
Bottom line on detox foods/drinks:
- Fiber is great; juicing removes fiber. Eat your greens (don’t drink them)!
- Activated charcoal is the heavy artillery of detoxing
- Sometimes it will remove things you didn’t want removed, though
- It also won’t help against alcohol, sadly
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: