Nicotine pouches are being marketed to young people on social media. But are they safe, or even legal?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Flavoured nicotine pouches are being promoted to young people on social media platforms such as TikTok and Instagram.
Although some viral videos have been taken down following a series of reports in The Guardian, clips featuring Australian influencers have claimed nicotine pouches are a safe and effective way to quit vaping. A number of the videos have included links to websites selling these products.
With the rapid rise in youth vaping and the subsequent implementation of several reforms to restrict access to vaping products, it’s not entirely surprising the tobacco industry is introducing more products to maintain its future revenue stream.
The major trans-national tobacco companies, including Philip Morris International and British American Tobacco, all manufacture nicotine pouches. British American Tobacco’s brand of nicotine pouches, Velo, is a leading sponsor of the McLaren Formula 1 team.
But what are nicotine pouches, and are they even legal in Australia?
Like snus, but different
Nicotine pouches are available in many countries around the world, and their sales are increasing rapidly, especially among young people.
Nicotine pouches look a bit like small tea bags and are placed between the lip and gum. They’re typically sold in small, colourful tins of about 15 to 20 pouches. While the pouches don’t contain tobacco, they do contain nicotine that is either extracted from tobacco plants or made synthetically. The pouches come in a wide range of strengths.
As well as nicotine, the pouches commonly contain plant fibres (in place of tobacco, plant fibres serve as a filler and give the pouches shape), sweeteners and flavours. Just like for vaping products, there’s a vast array of pouch flavours available including different varieties of fruit, confectionery, spices and drinks.
The range of appealing flavours, as well as the fact they can be used discreetly, may make nicotine pouches particularity attractive to young people.

Aleksandr Yu/Shutterstock
Users absorb the nicotine in their mouths and simply replace the pouch when all the nicotine has been absorbed. Tobacco-free nicotine pouches are a relatively recent product, but similar style products that do contain tobacco, known as snus, have been popular in Scandinavian countries, particularly Sweden, for decades.
Snus and nicotine pouches are however different products. And given snus contains tobacco and nicotine pouches don’t, the products are subject to quite different regulations in Australia.
What does the law say?
Pouches that contain tobacco, like snus, have been banned in Australia since 1991, as part of a consumer product ban on all forms of smokeless tobacco products. This means other smokeless tobacco products such as chewing tobacco, snuff, and dissolvable tobacco sticks or tablets, are also banned from sale in Australia.
Tobacco-free nicotine pouches cannot legally be sold by general retailers, like tobacconists and convenience stores, in Australia either. But the reasons for this are more complex.
In Australia, under the Poisons Standard, nicotine is a prescription-only medicine, with two exceptions. Nicotine can be used in tobacco prepared and packed for smoking, such as cigarettes, roll-your-own tobacco, and cigars, as well as in preparations for therapeutic use as a smoking cessation aid, such as nicotine patches, gum, mouth spray and lozenges.
If a nicotine-containing product does not meet either of these two exceptions, it cannot be legally sold by general retailers. No nicotine pouches have currently been approved by the Therapeutic Goods Administration as a therapeutic aid in smoking cessation, so in short they’re not legal to sell in Australia.
However, nicotine pouches can be legally imported for personal use only if users have a prescription from a medical professional who can assess if the product is appropriate for individual use.
We only have anecdotal reports of nicotine pouch use, not hard data, as these products are very new in Australia. But we do know authorities are increasingly seizing these products from retailers. It’s highly unlikely any young people using nicotine pouches are accessing them through legal channels.
Health concerns
Nicotine exposure may induce effects including dizziness, headache, nausea and abdominal cramps, especially among people who don’t normally smoke or vape.
Although we don’t yet have much evidence on the long term health effects of nicotine pouches, we know nicotine is addictive and harmful to health. For example, it can cause problems in the cardiovascular system (such as heart arrhythmia), particularly at high doses. It may also have negative effects on adolescent brain development.
The nicotine contents of some of the nicotine pouches on the market is alarmingly high. Certain brands offer pouches containing more than 10mg of nicotine, which is similar to a cigarette. According to a World Health Organization (WHO) report, pouches deliver enough nicotine to induce and sustain nicotine addiction.
Pouches are also being marketed as a product to use when it’s not possible to vape or smoke, such as on a plane. So instead of helping a person quit they may be used in addition to smoking and vaping. And importantly, there’s no clear evidence pouches are an effective smoking or vaping cessation aid.

Becky Freeman
Further, some nicotine pouches, despite being tobacco-free, still contain tobacco-specific nitrosamines. These compounds can damage DNA, and with long term exposure, can cause cancer.
Overall, there’s limited data on the harms of nicotine pouches because they’ve been on the market for only a short time. But the WHO recommends a cautious approach given their similarities to smokeless tobacco products.
For anyone wanting advice and support to quit smoking or vaping, it’s best to talk to your doctor or pharmacist, or access trusted sources such as Quitline or the iCanQuit website.
Becky Freeman, Associate Professor, School of Public Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
For Seniors With Hoarding Disorder, a Support Group Helps Confront Stigma and Isolation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A dozen people seated around folding tables clap heartily for a beaming woman: She’s donated two 13-gallon garbage bags full of clothes, including several Christmas sweaters and a couple of pantsuits, to a Presbyterian church.
A closet cleanout might not seem a significant accomplishment. But as the people in this Sunday-night class can attest, getting rid of stuff is agonizing for those with hoarding disorder.
People with the diagnosis accumulate an excessive volume of things such as household goods, craft supplies, even pets. In extreme cases, their homes become so crammed that moving between rooms is possible only via narrow pathways.
These unsafe conditions can also lead to strained relationships.
“I’ve had a few relatives and friends that have condemned me, and it doesn’t help,” said Bernadette, a Pennsylvania woman in her early 70s who has struggled with hoarding since retiring and no longer allows guests in her home.
People who hoard are often stigmatized as lazy or dirty. NPR, Spotlight PA, and KFF Health News agreed to use only the first names of people with hoarding disorder interviewed for this article because they fear personal and professional repercussions if their condition is made public.
As baby boomers age into the group most affected by hoarding disorder, the psychiatric condition is a growing public health concern. Effective treatments are scarce. And because hoarding can require expensive interventions that drain municipal resources, more funding and expertise is needed to support those with the diagnosis before the issue grows into a crisis.
For Bernadette, the 16-week course is helping her turn over a new leaf.
The program doubles as a support group and is provided through Fight the Blight. The Westmoreland County, Pennsylvania, organization started offering the course at a local Masonic temple after founder Matt Williams realized the area lacked hoarding-specific mental health services.
Fight the Blight uses a curriculum based on cognitive behavioral therapy to help participants build awareness of what fuels their hoarding. People learn to be more thoughtful about what they purchase and save, and they create strategies so that decluttering doesn’t become overwhelming.
Perhaps more importantly, attendees say they’ve formed a community knitted together through the shared experience of a psychiatric illness that comes with high rates of social isolation and depression.
“You get friendship,” said Sanford, a classmate of Bernadette’s.
After a lifetime of judgment, these friendships have become an integral part of the changes that might help participants eventually clear out the clutter.
Clutter Catches Up to Baby Boomers
Studies have estimated that hoarding disorder affects around 2.5% of the general population — a higher rate than schizophrenia.
The mental illness was previously considered a subtype of obsessive-compulsive disorder, but in 2013 it was given its own diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, the DSM-5.
The biological and environmental factors that may drive hoarding are not well understood. Symptoms usually appear during the teenage years and tend to be more severe among older adults with the disorder. That’s partly because they have had more time to acquire things, said Kiara Timpano, a University of Miami psychology professor.
“All of a sudden you have to downsize this huge home with all the stuff and so it puts pressures on individuals,” she said. In Bernadette’s case, her clutter includes a collection of VHS tapes, and spices in her kitchen that she said date back to the Clinton administration.
But it’s more than just having decades to stockpile possessions; the urge to accumulate strengthens with age, according to Catherine Ayers, a psychiatry professor at the University of California-San Diego.
Researchers are working to discern why. Ayers and Timpano theorize that age-related cognitive changes — particularly in the frontal lobe, which regulates impulsivity and problem-solving — might exacerbate the disorder.
“It is the only mental health disorder, besides dementia, that increases in prevalence and severity with age,” Ayers said.
As the U.S. population ages, hoarding presents a growing public health concern: Some 1 in 5 U.S. residents are baby boomers, all of whom will be 65 or older by 2030.
This population shift will require the federal government to address hoarding disorder, among other age-related issues that it has not previously prioritized, according to a July report by the Democratic staff of the U.S. Senate Special Committee on Aging, chaired then by former Sen. Bob Casey (D-Pa.).
Health Hazards of Hoarding
Clutter creates physical risks. A cramped and disorderly home is especially dangerous for older adults because the risk of falling and breaking a bone increases with age. And having too many things in one space can be a fire hazard.
Last year, the National Fallen Firefighters Foundation wrote to the Senate committee’s leadership that “hoarding conditions are among the most dangerous conditions the fire service can encounter.” The group also said that cluttered homes delay emergency care and increase the likelihood of a first responder being injured on a call.
The Bucks County Board of Commissioners in Pennsylvania told Casey that hoarding-related mold and insects can spread to adjacent households, endangering the health of neighbors.
Due to these safety concerns, it might be tempting for a family member or public health agency to quickly empty someone’s home in one fell swoop.
That can backfire, Timpano said, as it fails to address people’s underlying issues and can be traumatic.
“It can really disrupt the trust and make it even less likely that the individual is willing to seek help in the future,” she said.
It’s more effective, Timpano said, to help people build internal motivation to change and help them identify goals to manage their hoarding.
For example, at the Fight the Blight class, a woman named Diane told the group she wanted a cleaner home so she could invite people over and not feel embarrassed.
Sanford said he is learning to keep his documents and record collection more organized.
Bernadette wants to declutter her bedroom so she can start sleeping in it again. Also, she’s glad she cleared enough space on the first floor for her cat to play.
“Because now he’s got all this room,” she said, “he goes after his tail like a crazy person.”
Ultimately, the home of someone with hoarding disorder might always be a bit cluttered, and that’s OK. The goal of treatment is to make the space healthy and safe, Timpano said, not to earn Marie Kondo’s approval.
Lack of Treatment Leaves Few Options
A 2020 study found that hoarding correlates with homelessness, and those with the disorder are more likely to be evicted.
Housing advocates argue that under the Fair Housing Act, tenants with the diagnosis are entitled to reasonable accommodation. This might include allowing someone time to declutter a home and seek therapy before forcing them to leave their home.
But as outlined in the Senate aging committee’s report, a lack of resources limits efforts to carry out these accommodations.
Hoarding is difficult to treat. In a 2018 study led by Ayers, the UCSD psychiatrist, researchers found that people coping with hoarding need to be highly motivated and often require substantial support to remain engaged with their therapy.
The challenge of sticking with a treatment plan is exacerbated by a shortage of clinicians with necessary expertise, said Janet Spinelli, the co-chair of Rhode Island’s hoarding task force.
Could Changes to Federal Policy Help?
Casey, the former Pennsylvania senator, advocated for more education and technical assistance for hoarding disorder.
In September, he called for the Substance Abuse and Mental Health Services Administration to develop training, assistance, and guidance for communities and clinicians. He also said the Centers for Medicare & Medicaid Services should explore ways to cover evidence-based treatments and services for hoarding.
This might include increased Medicare funding for mobile crisis services to go to people’s homes, which is one way to connect someone to therapy, Spinelli said.
Another strategy would involve allowing Medicaid and Medicare to reimburse community health workers who assist patients with light cleaning and organizing; research has found that many who hoard struggle with categorization tasks.
Williams, of Fight the Blight, agrees that in addition to more mental health support, taxpayer-funded services are needed to help people address their clutter.
When someone in the group reaches a point of wanting to declutter their home, Fight the Blight helps them start the process of cleaning, removing, and organizing.
The service is free to those earning less than 150% of the federal poverty level. People making above that threshold can pay for assistance on a sliding scale; the cost varies also depending on the size of a property and severity of the hoarding.
Also, Spinelli thinks Medicaid and Medicare should fund more peer-support specialists for hoarding disorder. These mental health workers draw on their own life experiences to help people with similar diagnoses. For example, peer counselors could lead classes like Fight the Blight’s.
Bernadette and Sanford say courses like the one they enrolled in should be available all over the U.S.
To those just starting to address their own hoarding, Sanford advises patience and persistence.
“Even if it’s a little job here, a little job there,” he said, “that all adds up.”
This article is from a partnership that includes Spotlight PA, NPR, and KFF Health News.
Spotlight PA is an independent, nonpartisan, and nonprofit newsroom producing investigative and public-service journalism that holds power to account and drives positive change in Pennsylvania. Sign up for its free newsletters.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
How Primary Care Is Being Disrupted: A Video Primer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How patients are seeing their doctor is changing, and that could shape access to and quality of care for decades to come.
More than 100 million Americans don’t have regular access to primary care, a number that has nearly doubled since 2014. Yet demand for primary care is up, spurred partly by record enrollment in Affordable Care Act plans. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades.
KFF Health News senior correspondent Julie Appleby breaks down what is happening — and what it means for patients.
More From This Investigation
Primary Care Disrupted
Known as the “front door” to the health system, primary care is changing. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades. KFF Health News looks at what this means for patients.
Credits
Hannah Norman Video producer and animator Oona Tempest Illustrator and creative director KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Here’s the latest you need to know about bird flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Although bird flu continues to spread in wild birds, livestock, and humans, the risk to the public remains low.
- The majority of U.S. bird flu cases have been reported in farm workers who had direct contact with infected birds and cattle. Health officials are working to monitor the spread of the virus and improve protections for those most at risk.
- Recent data suggests that mutations in bird flu viruses could make them more dangerous to humans and potentially increase the risk of a pandemic.
- On January 6, Louisiana health officials confirmed the first U.S. death from bird flu.
Throughout 2024, dozens of human cases of H5N1 bird flu were detected as the virus spreads rapidly in livestock. The current risk to humans is low but not nonexistent. Here’s everything you need to know about the current status and future outlook of H5 bird flu in the United States.
Current U.S. bird flu status (as of January 6, 2025)
As of January 6, 66 human bird flu cases have been reported in eight states. Over half of all cases are in California. The state’s governor declared a state of emergency as a “proactive” action against bird flu on December 18.
On January 6, the Louisiana Department of Health reported the first U.S. bird flu death. The patient, a man over age 65, was previously confirmed to be the first severe bird flu case in the U.S. and the first case linked to backyard flocks. The department emphasized that the risk to the public is low and that no new cases or evidence of human transmission have been detected in the state.
All but two human bird flu cases this year were in farm workers who were exposed to infected livestock. The exposure source of the remaining cases—one in California and one in Missouri—is unknown.
The CDC reported on November 22 that a child in California tested positive for bird flu, the first known pediatric bird flu case in the U.S. However, it is unclear how the child contracted the virus, as they had no known contact with infected animals.
To date, there have been no reports of human transmission of bird flu during the current outbreak. Additionally, most human cases have not been severe, and no deaths have been reported. For these reasons, experts are confident that the bird flu risk to humans remains low.
“In the short term, there is very little threat,” Dr. Scott Roberts, an infectious diseases specialist with Yale Medicine said. “The risk for the general public is so low,” he emphasized to Yale Medicine.
How the U.S. is monitoring bird flu
The CDC continues to monitor the circulation of bird flu in humans as part of its year-round flu monitoring. The agency is also working to improve protections for farm workers, who are at the highest risk of contracting bird flu.
In November 2024, the CDC also announced expanded actions and updated guidance for farm workers, including improved access to and training for using personal protective equipment (such as N95 face masks), more rigorous testing procedures, and increased outreach. These updates followed a CDC report finding that 7 percent of participating dairy workers had signs of a recent bird flu infection. A second CDC study, also released in November, found inadequate use of personal protective equipment among dairy workers on farms with bird flu outbreaks.
After the H5N1 virus was found in raw milk being sold in California, the U.S. Department of Agriculture announced on December 6 that unpasteurized milk must be tested for bird flu. The USDA order also requires dairy farms with positive bird flu cases to cooperate with health officials in disease surveillance.
Is a bird flu pandemic possible?
In early November, a Canadian teen was hospitalized with bird flu caused by a virus that’s closely related to the H5N1 virus circulating in the U.S. The case has troubled experts for a few reasons.
First, it is Canada’s first human bird flu case where the patient was not infected while traveling, and the source of exposure is unknown. Second, the teen experienced severe symptoms and developed a lung infection requiring critical care, raising concern that bird flu infections may be more severe in younger people.
The final and biggest concern about the case is that genetic analysis revealed several changes in the virus’s DNA sequence, called mutations, that could potentially make the virus better able to infect humans. Researchers say that two of those mutations could make it easier for the virus to infect humans, and another one may make it easier for the virus to replicate after infecting a human. However, it’s unclear if the changes occurred before or after the teen was infected.
Scott Hensley, a professor of microbiology at the University of Pennsylvania, told Nature that “this should serve as a warning: this virus has the capacity to switch very quickly into a form that can cause severe disease.”
Notably, even in this more severe case, there is still no evidence of human transmission, which is necessary for a potential bird flu pandemic. However, the case underscores the risk of new and potentially dangerous mutations emerging as the H5N1 virus continues to spread and multiply.
A study published in Science on December 5 found that a genetic change on a protein on the surface of the virus could make it easier for the virus to attach to and infect human cells. But none of the mutations observed in the Canadian case are those identified in the study.
Importantly, the researchers stressed that the ability of the virus to attach to a specific part of human cells “is not the only [factor] required for human-to-human transmission of influenza viruses.”
How to stay safe
Most people are not at high risk of being exposed to bird flu. The virus is spreading between animals and from animals to humans through direct contact. The CDC recommends avoiding the consumption of raw milk products and direct contact with wild birds and potentially infected livestock.
“Pasteurization kills the bird flu virus and other harmful germs that can be found in raw milk,” says a November 24 California Department of Public Health press release. “CDPH advises consumers not to drink raw milk or eat raw milk products due to the risk of foodborne illnesses.”
Additionally, although the annual flu shot does not protect against bird flu, getting vaccinated helps prevent infection with seasonal flu and bird flu at the same time. In very rare instances, getting infected by two influenza viruses at the same time can result in a combination of genetic material that produces a new virus.
This phenomenon, known as antigenic shift, triggered the 2009 swine flu pandemic.
Learn more about how to protect yourself and your loved ones against bird flu.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
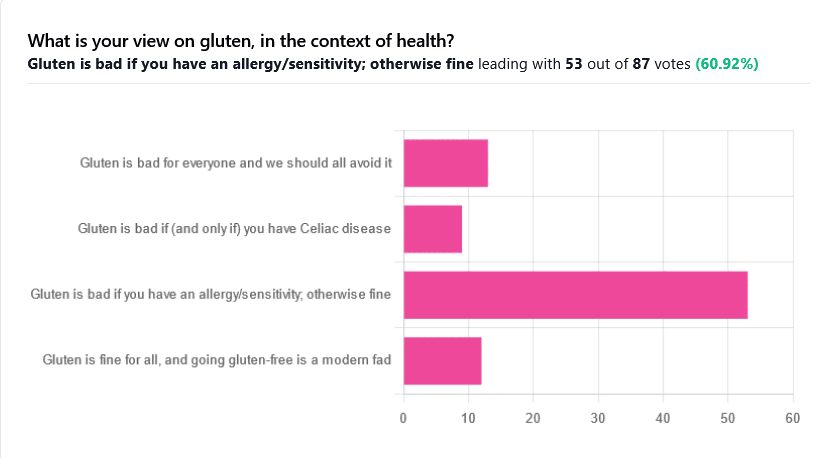
Gluten: What’s The Truth?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Gluten: What’s The Truth?
We asked you for your health-related view of gluten, and got the above spread of results. To put it simply:
Around 60% of voters voted for “Gluten is bad if you have an allergy/sensitivity; otherwise fine”
The rest of the votes were split fairly evenly between the other three options:
- Gluten is bad for everyone and we should avoid it
- Gluten is bad if (and only if) you have Celiac disease
- Gluten is fine for all, and going gluten-free is a modern fad
First, let’s define some terms so that we’re all on the same page:
What is gluten?
Gluten is a category of protein found in wheat, barley, rye, and triticale. As such, it’s not one single compound, but a little umbrella of similar compounds. However, for the sake of not making this article many times longer, we’re going to refer to “gluten” without further specification.
What is Celiac disease?
Celiac disease is an autoimmune disease. Like many autoimmune diseases, we don’t know for sure how/why it occurs, but a combination of genetic and environmental factors have been strongly implicated, with the latter putatively including overexposure to gluten.
It affects about 1% of the world’s population, and people with Celiac disease will tend to respond adversely to gluten, notably by inflammation of the small intestine and destruction of enterocytes (the cells that line the wall of the small intestine). This in turn causes all sorts of other problems, beyond the scope of today’s main feature, but suffice it to say, it’s not pleasant.
What is an allergy/intolerance/sensitivity?
This may seem basic, but a lot of people conflate allergy/intolerance/sensitivity, so:
- An allergy is when the body mistakes a harmless substance for something harmful, and responds inappropriately. This can be mild (e.g. allergic rhinitis, hayfever) or severe (e.g. peanut allergy), and as such, responses can vary from “sniffly nose” to “anaphylactic shock and death”.
- In the case of a wheat allergy (for example), this is usually somewhere between the two, and can for example cause breathing problems after ingesting wheat or inhaling wheat flour.
- An intolerance is when the body fails to correctly process something it should be able to process, and just ejects it half-processed instead.
- A common and easily demonstrable example is lactose intolerance. There isn’t a well-defined analog for gluten, but gluten intolerance is nonetheless a well-reported thing.
- A sensitivity is when none of the above apply, but the body nevertheless experiences unpleasant symptoms after exposure to a substance that should normally be safe.
- In the case of gluten, this is referred to as non-Celiac gluten sensitivity
A word on scientific objectivity: at 10almonds we try to report science as objectively as possible. Sometimes people have strong feelings on a topic, especially if it is polarizing.
Sometimes people with a certain condition feel constantly disbelieved and mocked; sometimes people without a certain condition think others are imagining problems for themselves where there are none.
We can’t diagnose anyone or validate either side of that, but what we can do is report the facts as objectively as science can lay them out.
Gluten is fine for all, and going gluten-free is a modern fad: True or False?
Definitely False, Celiac disease is a real autoimmune disease that cannot be faked, and allergies are also a real thing that people can have, and again can be validated in studies. Even intolerances have scientifically measurable symptoms and can be tested against nocebo.
See for example:
- Epidemiology and clinical presentations of Celiac disease
- Severe forms of food allergy that can precipitate allergic emergencies
- Properties of gluten intolerance: gluten structure, evolution, and pathogenicity
However! It may not be a modern fad, so much as a modern genuine increase in incidence.
Widespread varieties of wheat today contain a lot more gluten than wheat of ages past, and many other molecular changes mean there are other compounds in modern grains that never even existed before.
However, the health-related impact of these (novel proteins and carbohydrates) is currently still speculative, and we are not in the business of speculating, so we’ll leave that as a “this hasn’t been studied enough to comment yet but we recognize it could potentially be a thing” factor.
Gluten is bad if (and only if) you have Celiac disease: True or False?
Definitely False; allergies for example are well-evidenced as real; same facts as we discussed/linked just above.
Gluten is bad for everyone and we should avoid it: True or False?
False, tentatively and contingently.
First, as established, there are people with clinically-evidenced Celiac disease, wheat allergy, or similar. Obviously, they should avoid triggering those diseases.
What about the rest of us, and what about those who have non-Celiac gluten sensitivity?
Clinical testing has found that of those reporting non-Celiac gluten sensitivity, nocebo-controlled studies validate that diagnosis in only a minority of cases.
In the following study, for example, only 16% of those reporting symptoms showed them in the trials, and 40% of those also showed a nocebo response (i.e., like placebo, but a bad rather than good effect):
This one, on the other hand, found that positive validations of diagnoses were found to be between 7% and 77%, depending on the trial, with an average of 30%:
Re-challenge Studies in Non-celiac Gluten Sensitivity: A Systematic Review and Meta-Analysis
In other words: non-Celiac gluten sensitivity is a thing, and/but may be over-reported, and/but may be in some part exacerbated by psychosomatic effect.
Note: psychosomatic effect does not mean “imagining it” or “all in your head”. Indeed, the “soma” part of the word “psychosomatic” has to do with its measurable effect on the rest of the body.
For example, while pain can’t be easily objectively measured, other things, like inflammation, definitely can.
As for everyone else? If you’re enjoying your wheat (or similar) products, it’s well-established that they should be wholegrain for the best health impact (fiber, a positive for your health, rather than white flour’s super-fast metabolites padding the liver and causing metabolic problems).
Wheat itself may have other problems, for example FODMAPs, amylase trypsin inhibitors, and wheat germ agglutinins, but that’s “a wheat thing” rather than “a gluten thing”.
That’s beyond the scope of today’s main feature, but you might want to check out today’s featured book!
For a final scientific opinion on this last one, though, here’s what a respected academic journal of gastroenterology has to say:
From coeliac disease to noncoeliac gluten sensitivity; should everyone be gluten-free?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Red Cabbage vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red cabbage to cauliflower, we picked the cabbage.
Why?
In terms of macros, there’s no meaningful difference between them; they’re both mostly water with just enough fiber to hold them together, a small amount of carbs, and an even more trivial amount of protein. So, a tie on macros.
Looking at the vitamins, red cabbage has more of vitamins A, B1, B2, B6, C, E, and K, while cauliflower has more of vitamins B3, B5, B9, and choline. So, a 7:4 win for red cabbage.
In the category of minerals, red cabbage has more calcium, manganese, and iron, while cauliflower has more copper, phosphorus, and potassium. The margins of difference are comparable too, thus, a 3:3 tie on minerals.
It’s always worth taking a look at polyphenols for plants like these, but in this case, once again, there’s not much to set one above the other. However, it’s good to note also that despite them both being Brassica oleracea (same species, different cultivar), there isn’t much overlap in their polyphenol content, meaning they complement each other very well. In particular, red cabbage is a source of luteolin and quercetin, while cauliflower is a source of gallic acid and caffeic acid, for example.
Adding up the three ties and the one win for red cabbage, gives the cabbage the victory today—but do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Longevity Project – by Dr. Howard Friedman & Dr. Leslie Martin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most books on the topic of longevity focus on such things as diet and exercise, and indeed, those are of course important things. But what of psychological and sociological factors?
Dr. Friedman and Dr. Martin look at a landmark longitudinal study, following a large group of subjects from childhood into old age. Looking at many lifestyle factors and life events, they crunched the numbers to see what things really made the biggest impact on healthy longevity.
A strength of the book is that this study had a huge amount of data—a limitation of the book is that it often avoids giving that concrete data, preferring to say “many”, “a majority”, “a large minority”, “some”, and so forth.
However, the conclusions from the data seem clear, and include many observations such as:
- conscientiousness is a characteristic that not only promotes healthy long life, but also can be acquired as time goes by (some “carefree” children became “conscientious” adults)
- resilience is a characteristic that promotes healthy long life—but tends to only be “unlocked” by adversity
- men tend to live longer if married—women, not so much
- religion and spirituality are not big factors in healthy longevity—but social connections (that may or may not come with such) do make a big difference
Bottom line: if you’d like to know which of your decisions are affecting your healthy longevity (beyond the obvious diet, exercise, etc), this is a great book for collating that information and presenting, in essence, a guideline for a long healthy life.
Click here to check out The Longevity Project and see how it applies to your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: