New research suggests intermittent fasting increases the risk of dying from heart disease. But the evidence is mixed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Kaitlin Day, RMIT University and Sharayah Carter, RMIT University
Intermittent fasting has gained popularity in recent years as a dietary approach with potential health benefits. So you might have been surprised to see headlines last week suggesting the practice could increase a person’s risk of death from heart disease.
The news stories were based on recent research which found a link between time-restricted eating, a form of intermittent fasting, and an increased risk of death from cardiovascular disease, or heart disease.
So what can we make of these findings? And how do they measure up with what else we know about intermittent fasting and heart disease?
The study in question
The research was presented as a scientific poster at an American Heart Association conference last week. The full study hasn’t yet been published in a peer-reviewed journal.
The researchers used data from the National Health and Nutrition Examination Survey (NHANES), a long-running survey that collects information from a large number of people in the United States.
This type of research, known as observational research, involves analysing large groups of people to identify relationships between lifestyle factors and disease. The study covered a 15-year period.
It showed people who ate their meals within an eight-hour window faced a 91% increased risk of dying from heart disease compared to those spreading their meals over 12 to 16 hours. When we look more closely at the data, it suggests 7.5% of those who ate within eight hours died from heart disease during the study, compared to 3.6% of those who ate across 12 to 16 hours.
We don’t know if the authors controlled for other factors that can influence health, such as body weight, medication use or diet quality. It’s likely some of these questions will be answered once the full details of the study are published.
It’s also worth noting that participants may have eaten during a shorter window for a range of reasons – not necessarily because they were intentionally following a time-restricted diet. For example, they may have had a poor appetite due to illness, which could have also influenced the results.
Other research
Although this research may have a number of limitations, its findings aren’t entirely unique. They align with several other published studies using the NHANES data set.
For example, one study showed eating over a longer period of time reduced the risk of death from heart disease by 64% in people with heart failure.
Another study in people with diabetes showed those who ate more frequently had a lower risk of death from heart disease.
A recent study found an overnight fast shorter than ten hours and longer than 14 hours increased the risk dying from of heart disease. This suggests too short a fast could also be a problem.
But I thought intermittent fasting was healthy?
There are conflicting results about intermittent fasting in the scientific literature, partly due to the different types of intermittent fasting.
There’s time restricted eating, which limits eating to a period of time each day, and which the current study looks at. There are also different patterns of fast and feed days, such as the well-known 5:2 diet, where on fast days people generally consume about 25% of their energy needs, while on feed days there is no restriction on food intake.
Despite these different fasting patterns, systematic reviews of randomised controlled trials (RCTs) consistently demonstrate benefits for intermittent fasting in terms of weight loss and heart disease risk factors (for example, blood pressure and cholesterol levels).
RCTs indicate intermittent fasting yields comparable improvements in these areas to other dietary interventions, such as daily moderate energy restriction.

So why do we see such different results?
RCTs directly compare two conditions, such as intermittent fasting versus daily energy restriction, and control for a range of factors that could affect outcomes. So they offer insights into causal relationships we can’t get through observational studies alone.
However, they often focus on specific groups and short-term outcomes. On average, these studies follow participants for around 12 months, leaving long-term effects unknown.
While observational research provides valuable insights into population-level trends over longer periods, it relies on self-reporting and cannot demonstrate cause and effect.
Relying on people to accurately report their own eating habits is tricky, as they may have difficulty remembering what and when they ate. This is a long-standing issue in observational studies and makes relying only on these types of studies to help us understand the relationship between diet and disease challenging.
It’s likely the relationship between eating timing and health is more complex than simply eating more or less regularly. Our bodies are controlled by a group of internal clocks (our circadian rhythm), and when our behaviour doesn’t align with these clocks, such as when we eat at unusual times, our bodies can have trouble managing this.
So, is intermittent fasting safe?
There’s no simple answer to this question. RCTs have shown it appears a safe option for weight loss in the short term.
However, people in the NHANES dataset who eat within a limited period of the day appear to be at higher risk of dying from heart disease. Of course, many other factors could be causing them to eat in this way, and influence the results.
When faced with conflicting data, it’s generally agreed among scientists that RCTs provide a higher level of evidence. There are too many unknowns to accept the conclusions of an epidemiological study like this one without asking questions. Unsurprisingly, it has been subject to criticism.
That said, to gain a better understanding of the long-term safety of intermittent fasting, we need to be able follow up individuals in these RCTs over five or ten years.
In the meantime, if you’re interested in trying intermittent fasting, you should speak to a health professional first.
Kaitlin Day, Lecturer in Human Nutrition, RMIT University and Sharayah Carter, Lecturer Nutrition and Dietetics, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chew On This… But Don’t Swallow − by Dr. Blanche Grube & Anita Vasquez-Tibau
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Blanche Grube is a dentist with over 40 years of experience, and Anita Vasquez-Tibau is a well-respected research scientist with many peer-reviewed publications to her name, and both have lectured extensively.
So, what do they want us to know?
It’s mostly about the iatrogenic (i.e., caused by treatment) harm done by many common conventional dental practices (including dental mercury amalgams, metal crowns, root canals, implants, and even braces), and how we can avoid such, and enjoy better treatment instead.
After an introductory overview of the basics (and also where her own work came from in the first place, namely, her own root canals that were established as largely responsible for her leukemia), the largest part of the book is practical advice, laid out practically. What things come with what risks, what things get advertised differently than they really are, and which way to go in the case of unenviable situations where one must choose the “least bad” option out of a bunch of bad options.
Lastly, she discusses a range of solutions that can help side-step most problems, provided one implements them early. The good news is, they are “do these small things every day” recommendations, not “get this prophylactic surgical treatment” options. And yes, they are beyond the obvious of good dental hygiene, though she does cover that too.
The style is in part narrative, in part explanatory, and/but very readable throughout.
Bottom line: if you love having teeth and/but don’t love going to the dentist, this book will help you take good care of yourself, and also mean you can safely and informedly advocate for yourself if you do find yourself in the dentist’s office.
Click here to check out Chew On This… But Don’t Swallow, and protect your teeth!
Share This Post
-
How much weight do you actually need to lose? It might be a lot less than you think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re one of the one in three Australians whose New Year’s resolution involved losing weight, it’s likely you’re now contemplating what weight-loss goal you should actually be working towards.
But type “setting a weight loss goal” into any online search engine and you’ll likely be left with more questions than answers.
Sure, the many weight-loss apps and calculators available will make setting this goal seem easy. They’ll typically use a body mass index (BMI) calculator to confirm a “healthy” weight and provide a goal weight based on this range.
Your screen will fill with trim-looking influencers touting diets that will help you drop ten kilos in a month, or ads for diets, pills and exercise regimens promising to help you effortlessly and rapidly lose weight.
Most sales pitches will suggest you need to lose substantial amounts of weight to be healthy – making weight loss seem an impossible task. But the research shows you don’t need to lose a lot of weight to achieve health benefits.
Using BMI to define our target weight is flawed
We’re a society fixated on numbers. So it’s no surprise we use measurements and equations to score our weight. The most popular is BMI, a measure of our body weight-to-height ratio.
BMI classifies bodies as underweight, normal (healthy) weight, overweight or obese and can be a useful tool for weight and health screening.
But it shouldn’t be used as the single measure of what it means to be a healthy weight when we set our weight-loss goals. This is because it:
- fails to consider two critical factors related to body weight and health – body fat percentage and distribution
- does not account for significant differences in body composition based on gender, ethnicity and age.
How does losing weight benefit our health?
Losing just 5–10% of our body weight – between 6 and 12kg for someone weighing 120kg – can significantly improve our health in four key ways.
1. Reducing cholesterol
Obesity increases the chances of having too much low-density lipoprotein (LDL) cholesterol – also known as bad cholesterol – because carrying excess weight changes how our bodies produce and manage lipoproteins and triglycerides, another fat molecule we use for energy.
Having too much bad cholesterol and high triglyceride levels is not good, narrowing our arteries and limiting blood flow, which increases the risk of heart disease, heart attack and stroke.
But research shows improvements in total cholesterol, LDL cholesterol and triglyceride levels are evident with just 5% weight loss.
2. Lowering blood pressure
Our blood pressure is considered high if it reads more than 140/90 on at least two occasions.
Excess weight is linked to high blood pressure in several ways, including changing how our sympathetic nervous system, blood vessels and hormones regulate our blood pressure.
Essentially, high blood pressure makes our heart and blood vessels work harder and less efficiently, damaging our arteries over time and increasing our risk of heart disease, heart attack and stroke.
Losing weight can lower your blood pressure.
Prostock-studio/ShutterstockLike the improvements in cholesterol, a 5% weight loss improves both systolic blood pressure (the first number in the reading) and diastolic blood pressure (the second number).
A meta-analysis of 25 trials on the influence of weight reduction on blood pressure also found every kilo of weight loss improved blood pressure by one point.
3. Reducing risk for type 2 diabetes
Excess body weight is the primary manageable risk factor for type 2 diabetes, particularly for people carrying a lot of visceral fat around the abdomen (belly fat).
Carrying this excess weight can cause fat cells to release pro-inflammatory chemicals that disrupt how our bodies regulate and use the insulin produced by our pancreas, leading to high blood sugar levels.
Type 2 diabetes can lead to serious medical conditions if it’s not carefully managed, including damaging our heart, blood vessels, major organs, eyes and nervous system.
Research shows just 7% weight loss reduces risk of developing type 2 diabetes by 58%.
4. Reducing joint pain and the risk of osteoarthritis
Carrying excess weight can cause our joints to become inflamed and damaged, making us more prone to osteoarthritis.
Observational studies show being overweight doubles a person’s risk of developing osteoarthritis, while obesity increases the risk fourfold.
Small amounts of weight loss alleviate this stress on our joints. In one study each kilogram of weight loss resulted in a fourfold decrease in the load exerted on the knee in each step taken during daily activities.
Losing weight eases stress on joints.
Shutterstock/Rostislav_SedlacekFocus on long-term habits
If you’ve ever tried to lose weight but found the kilos return almost as quickly as they left, you’re not alone.
An analysis of 29 long-term weight-loss studies found participants regained more than half of the weight lost within two years. Within five years, they regained more than 80%.
When we lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Just as the problem is evolutionary, the solution is evolutionary too. Successfully losing weight long-term comes down to:
losing weight in small manageable chunks you can sustain, specifically periods of weight loss, followed by periods of weight maintenance, and so on, until you achieve your goal weight
making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
Setting a goal to reach a healthy weight can feel daunting. But it doesn’t have to be a pre-defined weight according to a “healthy” BMI range. Losing 5–10% of our body weight will result in immediate health benefits.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How they did it: STAT reporters expose how ailing seniors suffer when Medicare Advantage plans use algorithms to deny care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a call with a long-time source, what stood out most to STAT reporters Bob Herman and Casey Ross was just how viscerally frustrated and angry the source was about an algorithm used by insurance companies to decide how long patients should stay in a nursing home or rehab facility before being sent home.
The STAT stories had a far-reaching impact:
- The U.S. Senate Committee on Homeland Security and Government Affairs took a rare step of launching a formal investigation into the use of algorithms by the country’s three largest Medicare Advantage insurers.
- Thirty-two House members urged the Centers for Medicare and Medicaid Services to increase the oversight of algorithms that health insurers use to make coverage decisions.
- In a rare step, CMS launched its own investigation into UnitedHealth. It also stiffened its regulations on the use of proprietary algorithms and introduced plans to audit denials across Medicare Advantage plans in 2024.
- Based on STAT’s reporting, Medicare Advantage beneficiaries filed two class-action lawsuits against UnitedHealth and its NaviHealth subsidiary, the maker of the algorithm, and against Humana, another major health insurance company that was also using the algorithm.
- Amid scrutiny, UnitedHealth renamed NaviHealth.
The companies never allowed an on-the-record interview with their executives, but they acknowledged that STAT’s reporting was true, according to the news organization.
Ross and Herman spoke with The Journalist’s Resource about their project and shared the following eight tips.
1. Search public comments on proposed federal rules to find sources.
Herman and Ross knew that the Centers for Medicare and Medicaid Services had put out a request for public comments, asking stakeholders within the Medicare Advantage industry how the system could improve.
There are two main ways to get Medicare coverage: original Medicare, which is a fee-for-service health plan, and Medicare Advantage, which is a type of Medicare health plan offered by private insurance companies that contract with Medicare. Medicare Advantage plans have increasingly become popular in recent years.
Under the Social Security Act, the public has the opportunity to submit comments on Medicare’s proposed national coverage determinations. CMS uses public comments to inform its proposed and final decisions. It responds in detail to all public comments when issuing a final decision.
The reporters began combing through hundreds of public comments attached to a proposed Medicare Advantage rule that was undergoing federal review. NaviHealth, the UnitedHealth subsidiary and the maker of the algorithm, came up in many of the comments, which include the submitters’ information.
“These are screaming all-caps comments to federal regulators about YOU NEED TO SOMETHING ABOUT THIS BECAUSE IT’S DISGUSTING,” Ross says.
“The federal government is proposing rules and regulations all the time,” adds Herman, STAT’s business of health care reporter. “If someone’s going to take the time and effort to comment on them, they must have at least some knowledge of what’s going on. It’s just a great tool for any journalist to use to figure out more and who to contact.”
The reporters also found several attorneys who had complained in the comments. They began reaching out to them, eventually gaining access to confidential documents and intermediaries who put them in touch with patients to show the human impact of the algorithm.
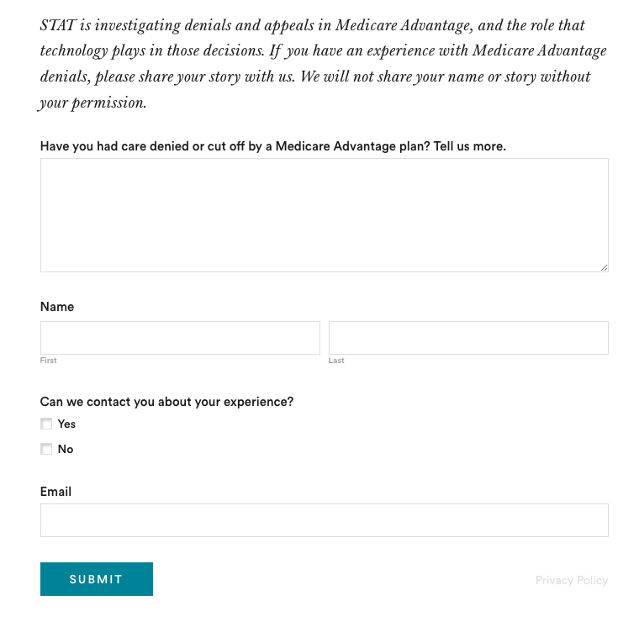
2. Harness the power of the reader submission box.
At the suggestion of an editor, the reporters added a reader submission box at the bottom of their first story, asking them to share their own experiences with Medicare Advantage denials.
The floodgates opened. Hundreds of submissions arrived.
By the end of their first story, Herman and Ross had confidential records and some patients, but they had no internal sources in the companies they were investigating, including Navihealth. The submission box led them to their first internal source.
(Screenshot of STAT’s submission box.) The journalists also combed through LinkedIn and reached out to former and current employees, but the response rate was much lower than what they received via the submission box.
The submission box “is just right there,” Herman says. “People who would want to reach out to us can do it right then and there after they read the story and it’s fresh in their minds.”
3. Mine podcasts relevant to your story.
The reporters weren’t sure if they could get interviews with some of the key figures in the story, including Tom Scully, the former head of the Centers for Medicare and Medicaid Services who drew up the initial plans for NaviHealth years before UnitedHealth acquired it.
But Herman and another colleague had written previously about Scully’s private equity firm and they had found a podcast where he talked about his work. So Herman went back to the podcast — where he discovered Scully had also discussed NaviHealth.
The reporters also used the podcast to get Scully on the phone for an interview.
“So we knew we had a good jumping off point there to be like, ‘OK, you’ve talked about NaviHealth on a podcast, let’s talk about this,’” Herman says. “I think that helped make him more willing to speak with us.”
4. When covering AI initiatives, proceed with caution.
“A source of mine once said to me, ‘AI is not magic,’” Ross says. “People need to just ask questions about it because AI has this aura about it that it’s objective, that it’s accurate, that it’s unquestionable, that it never fails. And that is not true.”
AI is not a neutral, objective machine, Ross says. “It’s based on data that’s fed into it and people need to ask questions about that data.”
He suggests several questions to ask about the data behind AI tools:
- Where does the data come from?
- Who does it represent?
- How is this tool being applied?
- Do the people to whom the tool is being applied match the data on which it was trained? “If racial groups or genders or age of economic situations are not adequately represented in the training set, then there can be an awful lot of bias in the output of the tool and how it’s applied,” Ross says.
- How is the tool applied within the institution? Are people being forced to forsake their judgment and their own ability to do their jobs to follow the algorithm?
5. Localize the story.
More than half of all Medicare beneficiaries have Medicare Advantage and there’s a high likelihood that there are multiple Medicare Advantage plans in every county across the nation.
“So it’s worth looking to see how Medicare Advantage plans are growing in your area,” Herman says.
Finding out about AI use will most likely rely on shoe-leather reporting of speaking with providers, nursing homes and rehab facilities, attorneys and patients in your community, he says. Another source is home health agencies, which may be caring for patients who were kicked out of nursing homes and rehab facilities too soon because of a decision by an algorithm.
The anecdote that opens their first story involves a small regional health insurer in Wisconsin, which was using NaviHealth and a contractor to manage post-acute care services, Ross says.
“It’s happening to people in small communities who have no idea that this insurer they’ve signed up with is using this tool made by this other company that operates nationally,” Ross says.
There are also plenty of other companies like NaviHealth that are being used by Medicare Advantage plans, Herman says. “So it’s understanding which Medicare Advantage plans are being sold in your area and then which post-acute management companies they’re using,” he adds.
Some regional insurers have online documents that show which contractors they use to evaluate post-acute care services.
6. Get familiar with Medicare’s appeals databases
Medicare beneficiaries can contest Medicare Advantage denials through a five-stage process, which can last months to years. The appeals can be filed via the Office of Medicare Hearings and Appeals.
“Between 2020 and 2022, the number of appeals filed to contest Medicare Advantage denials shot up 58%, with nearly 150,000 requests to review a denial filed in 2022, according to a federal database,” Ross and Herman write in their first story. “Federal records show most denials for skilled nursing care are eventually overturned, either by the plan itself or an independent body that adjudicates Medicare appeals.”
There are several sources to find appeals data. Be mindful that the cases themselves are not public to protect patient privacy, but you can find the number of appeals filed and the rationale for decisions.
CMS has two quality improvement organizations, or QIOs, Livanta and Kepro, which are required to file free, publicly-available annual reports, about the cases they handle, Ross says.
Another company, Maximus, a Quality Improvement Contractor, also files reports on prior authorization cases it adjudicates for Medicare. The free annual reports include data on raw numbers of cases and basic information about the percentage denials either overturned or upheld on appeal, Ross explains.
CMS also maintains its own database on appeals for Medicare Part C (Medicare Advantage plans) and Part D, which covers prescription drugs, although the data is not complete, Ross explains.
7. Give your editor regular updates.
“Sprinkle the breadcrumbs in front of your editors,” Ross says.
“If you wrap your editors in the process, you’re more likely to be able to get to the end of [the story] before they say, ‘That’s it! Give me your copy,’” Ross says.
8. Get that first story out.
“You don’t have to know everything before you write that first story,” Ross says. “Because with that first story, if it has credibility and it resonates with people, sources will come forward and sources will continue to come forward.”
Read the stories
Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need
UnitedHealth pushed employees to follow an algorithm to cut off Medicare patients’ rehab care
UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Genital herpes is on the rise. Here’s what to know about this common infection
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization (WHO) recently released new estimates suggesting around 846 million people aged between 15 and 49 live with a genital herpes infection.
That’s equivalent to one in every five people from that age group.
At least one person each second (42 million people annually) contracts a new genital herpes infection.
So what is genital herpes, and are cases on the rise? Here’s what to know about this common infection.
Peakstock/Shutterstock First, what causes genital herpes?
Genital herpes is a sexually transmitted infection (STI) caused by the herpes simplex virus, which also causes cold sores.
There are two types of herpes simplex virus, HSV-1 and HSV-2 (and it’s possible to be infected by both at the same time).
HSV-1 most commonly spreads through oral contact such as kissing or sharing infected objects such as lip balm, cups or utensils, and presents as cold sores (or oral herpes) around the mouth. But it can also be sexually transmitted to cause a genital herpes infection.
An estimated 3.8 billion people under the age of 50 (64%) globally have HSV-1.
HSV-2 is less prevalent, but almost always causes a genital herpes infection. Some 520 million people aged 15–49 (13%) worldwide are believed to have HSV-2.
The initial episode of genital herpes can be quite painful, with blisters, ulcers and peeling skin around the genitals over 7–10 days.
Not all people have severe (or any) initial symptoms. This means a person might not know they have been infected with a herpes virus.
Herpes is a lifelong infection, which means once you contract the virus, you have it forever. After an initial episode, subsequent episodes can occur, but are usually less painful or even symptom free.
Both oral and genital herpes are particularly easy to spread when you have active lesions (cold sores or genital ulcers). But even with no symptoms, herpes can still be spread to a partner.
And although relatively rare, oral herpes can be transmitted to the genital area, and genital herpes can be transmitted to the mouth through oral sex.
If an expectant mother exhibits a genital herpes infection close to childbirth, there are risks to the baby. A herpes infection can be very serious in a baby, and the younger the infant, the more vulnerable they are. This is also one reason why you should avoid kissing a baby on the mouth.
Changing trends
WHO’s recent figures brought together data from around the world to estimate the prevalence of genital herpes in 2020, compared with previous estimates in 2012 and 2016.
This data shows no significant difference in the prevalence of genital herpes caused by HSV-2 since 2016, but does highlight increases in genital herpes infections caused by HSV-1.
The estimated number of genital HSV-1 infections globally was nearly twice as high in 2020 compared with 2016 (376 million compared with 192 million).
A 2022 study looking at Australia, New Zealand and Canada found more than 60% of genital herpes infections are still caused by HSV-2. But this is declining by about 2% each year while new genital infections that result from HSV-1 are rising.
Genital herpes can be quite painful, presenting as sores and lesions that in severe cases, may take up to a month to fully heal. Christian Moro There’s no simple fix, but safe sex is important
Genital herpes causes a substantial disease burden and economic cost to health-care services.
With such a large proportion of the world’s population infected with HSV-1, evidence this virus is increasingly causing genital herpes is concerning.
There’s no cure for genital herpes, but some medications, such as antivirals, can help reduce the amount of virus present in the system. While this won’t kill it completely, it helps to prevent symptomatic genital herpes recurrences, improve quality of life, and minimise the risk of transmission.
To prevent the spread of genital herpes and other STIs, practise safe sex, particularly if you’re not sure of your partner’s sexual health. You need to use a barrier method such as condoms to protect against STIs (a contraceptive such as the pill won’t work). This includes during oral sex.
As herpes is now so common, testing is not usually included as part of a regular sexual health check-up, except for in specific circumstances such as during pregnancy or severe episodes.
So it’s wise not to let your guard down, even if your partner insists they have received the all-clear from a recent check-up.
If there are herpes lesions present around the genitals, avoid sex entirely. Even condoms are not fully effective at these times, as exposed areas can still transmit the infection.
Practising safe sex can help prevent the spread of herpes. cottonbro studio/Pexels Immune health
If you are infected with HSV-1 or HSV-2 it’s more likely symptoms will appear when you’re stressed, tired or overwhelmed. During these times, our immune system may not be as functional, and dormant viruses such as herpes can start to develop quickly in our bodies.
To reduce the risk of recurrent herpes infections, try to eat healthily, get at least seven hours of sleep each night if possible, and look out for when your body may be telling you to take a step back and relax. This self-care can go a long way towards keeping latent viruses at bay.
While the prevalence has increased significantly in recent years, we have not lost the war on genital herpes just yet. Safe sexual practices, education and awareness can help reduce its spread, and the stigma around it.
If you have personal concerns, you should discuss them with a medical professional.
Christian Moro, Associate Professor of Science & Medicine, Bond University and Charlotte Phelps, Senior Teaching Fellow in Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Many Faces Of Cosmetic Surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cosmetic Surgery: What’s The Truth?
In Tuesday’s newsletter, we asked you your opinion on elective cosmetic surgeries, and got the above-depicted, below-described, set of responses:
- About 48% said “Everyone should be able to get what they want, assuming informed consent”
- About 28% said “It can ease discomfort to bring features more in line with normalcy”
- 15% said “They should be available in the case of extreme disfigurement only”
- 10% said “No elective cosmetic surgery should ever be performed; needless danger”
Well, there was a clear gradient of responses there! Not so polarizing as we might have expected, but still enough dissent for discussion
So what does the science say?
The risks of cosmetic surgery outweigh the benefits: True or False?
False, subjectively (but this is important).
You may be wondering: how is science subjective?
And the answer is: the science is not subjective, but people’s cost:worth calculations are. What’s worth it to one person absolutely may not be worth it to another. Which means: for those for whom it wouldn’t be worth it, they are usually the people who will not choose the elective surgery.
Let’s look at some numbers (specifically, regret rates for various surgeries, elective/cosmetic or otherwise):
- Regret rate for elective cosmetic surgery in general: 20%
- Regret rate for knee replacement (i.e., not cosmetic): 17.1%
- Regret rate for hip replacement (i.e., not cosmetic): 4.8%
- Regret rate for gender-affirming surgeries (for transgender patients): 1%
So we can see, elective surgeries have an 80–99% satisfaction rate, depending on what they are. In comparison, the two joint replacements we mentioned have a 82.9–95.2% satisfaction rate. Not too dissimilar, taken in aggregate!
In other words: if a person has studied the risks and benefits of a surgery and decides to go ahead, they’re probably going to be happy with the results, and for them, the benefits will have outweighed the risks.
Sources for the above numbers, by the way:
- What is the regret rate for plastic surgery?
- Decision regret after primary hip and knee replacement surgery
- A systematic review of patient regret after surgery—a common phenomenon in many specialties but rare within gender-affirmation surgery
But it’s just a vanity; therapy is what’s needed instead: True or False?
False, generally. True, sometimes. Whatever the reasons for why someone feels the way they do about their appearance—whether their face got burned in a fire or they just have triple-J cups that they’d like reduced, it’s generally something they’ve already done a lot of thinking about. Nevertheless, it does also sometimes happen that it’s a case of someone hoping it’ll be the magical solution, when in reality something else is also needed.
How to know the difference? One factor is whether the surgery is “type change” or “restorative”, and both have their pros and cons.
- In “type change” (e.g. rhinoplasty), more psychological adjustment is needed, but when it’s all over, the person has a new nose and, statistically speaking, is usually happy with it.
- In “restorative” (e.g. facelift), less psychological adjustment is needed (as it’s just a return to a previous state), so a person will usually be happy quickly, but ultimately it is merely “kicking the can down the road” if the underlying problem is “fear of aging”, for example. In such a case, likely talking therapy would be beneficial—whether in place of, or alongside, cosmetic surgery.
Here’s an interesting paper on that; the sample sizes are small, but the discussion about the ideas at hand is a worthwhile read:
Does cosmetic surgery improve psychosocial wellbeing?
Some people will never be happy no matter how many surgeries they get: True or False?
True! We’re going to refer to the above paper again for this one. In particular, here’s what it said about one group for whom surgeries will not usually be helpful:
❝There is a particular subgroup of people who appear to respond poorly to cosmetic procedures. These are people with the psychiatric disorder known as “body dysmorphic disorder” (BDD). BDD is characterised by a preoccupation with an objectively absent or minimal deformity that causes clinically significant distress or impairment in social, occupational, or other areas of functioning.
For several reasons, it is important to recognise BDD in cosmetic surgery settings:
Firstly, it appears that cosmetic procedures are rarely beneficial for these people. Most patients with BDD who have had a cosmetic procedure report that it was unsatisfactory and did not diminish concerns about their appearance.
Secondly, BDD is a treatable disorder. Serotonin-reuptake inhibitors and cognitive behaviour therapy have been shown to be effective in about two-thirds of patients with BDD❞
~ Dr. David Castle et al. (lightly edited for brevity)
Which is a big difference compared to, for example, someone having triple-J breasts that need reducing, or the wrong genitals for their gender, or a face whose features are distinct outliers.
Whether that’s a reason people with BDD shouldn’t be able to get it is an ethical question rather than a scientific one, so we’ll not try to address that with science.
After all, many people (in general) will try to fix their woes with a haircut, a tattoo, or even a new sportscar, and those might sometimes be bad decisions, but they are still the person’s decision to make.
And even so, there can be protectionist laws/regulations that may provide a speed-bump, for example:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is silicosis and what does research say about it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Silicosis is a progressive, debilitating and sometimes fatal lung disease caused by breathing silica dust from cutting, drilling, chipping or grinding materials such as granite, sandstone, slate or artificial stone. The dust gets trapped in the lung tissue, causing inflammation, scarring and permanent damage.
Silicosis is a job-related lung disease and has no cure. The disease mostly affects workers in construction, stone countertop fabrication, mining, and even those who sandblast and stonewash denim jeans to create a ‘worn out’ look.
Silica is one of the most common minerals in nature. About 59% of the Earth’s crust is made of silica, found in quartz, granite, sandstone, slate and sand. Historically, people at the highest risk for the disease have worked in natural environments — mining, digging tunnels or doing quarry work. The disease was first documented by the Greek physician Hippocrates, who in 430 B.C. described breathing disorders in metal diggers.
But in recent decades there’s been renewed attention to the disease due to its more rapid progression and severity among younger workers. Research has shown that the culprit is artificial stone mostly used for countertops for kitchens and bathrooms, which has a very high silica content.
The new generation of coal miners is also at an increased risk of silicosis, in addition to black lung, because layers of coal have become thinner, forcing them to dig deeper into rock, as explained in a joint investigation by the Pittsburgh Post-Gazette and the Medill Investigative Lab at Northwestern University published on Dec. 4. CBS Sunday Morning also had a report on the same issue among West Virginia coal miners, aired as part of its Dec. 10 episode.
Silicosis in modern industries
Artificial, or engineered, stone used for countertops, also known as “quartz,” is formed from finely crushed rocks mixed with resin. Quartz is a natural mineral, but man-made products like many quartz countertops consist of not just quartz, but also resin, colors and other materials that are used to style and strengthen them.
The silica content of artificial stone is about 90%, compared with the 3% silica content of natural marble and 30% silica content in granite stones, according to the authors of a 2019 systematic review published in the International Journal of Environmental Research and Public Health.
The first reported case of silicosis associated with working with artificial stone was from Italy in 2010, according to a 2020 study published in Allergy. Since then, more studies have documented the growing number of cases among artificial stone workers, many of whom are from marginalized populations, such as immigrants.
A July 2023 study published in JAMA Internal Medicine found that in California, the disease mainly occurred among young Latino immigrant men. The disease was severe in most men by the time they sought care.
An August 2022 study, published in Occupational & Environmental Medicine, analyzing the Global Silicosis Registry, with workers in Israel, Spain, Australia and the U.S., found “a substantial emerging population of workers worldwide with severe and irreversible silica-associated diseases,” due to exposure from silica dust from engineered stone.
Other modern occupations such as denim sandblasting, work on dental prostheses, manufacturing of electrical cables and working on jewelry and semi-precious stones also put workers at risk of silicosis.
In the wake of modern-day silicosis cases, researchers have called for larger studies to better understand the disease and the discovery of effective treatments.
In the U.S. about 2.3 million workers are exposed to silica dust on the job, according to the American Lung Association. Other estimates show approximately 10 million workers in India, 3.2 million in the European Union and 2 million in Brazil work with material containing silica.
However, “the reporting system for occupational injuries and illnesses in the United States fails to capture many cases, leading to a poor understanding of silicosis incidence and prevalence,” writes Ryan F. Hoy, who has published extensively on the topic, in a June 2022 article in Respirology.
A 2015 study in the Morbidity & Mortality Weekly Report found the annual number of silicosis deaths declined from 185 people in 1999 to 111 in 2013, but the decline appeared to have leveled off between 2010 and 2013, the authors write. Another 2015 study in MMWR, examining silicosis deaths between 2001 and 2010, found the death rate from silicosis was significantly higher among Black people compared with whites and other races. Men also have a significantly higher death rate from silicosis than women.
The 2019 Global Burden of Disease Study estimates that more than 12,900 people worldwide die from silicosis each year.
Silicosis has no cure, but it’s preventable when workers have access to proper respiratory protection and are educated on safe practices set by regulatory bodies such as the U.S. National Institute for Occupational Safety and Health. The European Network on Silica also has guidelines on handling and using materials containing silica. A March 2023 study published in Environmental Science and Pollution Research International finds that “education, training, and marketing strategies improve respirator use, while training and education motivate workers to use dust control measures.”
Silicosis symptoms and treatment
Symptoms of silicosis include cough, fatigue, shortness of breath and chest pain. There’s no specific test for silicosis. The first signs may show in an abnormal chest X-ray and a slowly developing cough, according to the American Lung Association.
Silicosis symptoms don’t appear right away in most cases, usually taking several years to develop working with silica dust. However, studies indicate that symptoms of silicosis due to exposure to artificial stone appear quicker than exposure to natural silica sources, potentially due to the higher concentration of silica in artificial stone.
There are three types of silicosis: acute (most commonly caused by working with artificial stone), accelerated and chronic, depending on the level of exposure to silica dust, according to the Centers for Disease Control and Prevention, which explains the severity of each type on its website.
Complications from silicosis can include tuberculosis, lung cancer, chronic bronchitis, kidney disease and autoimmune disorders. In some cases, silicosis can cause severe scarring of the lung tissue, leading to a condition called progressive massive fibrosis, or PMF. Some patients may require a lung transplant.
Lung damage from silicosis is irreversible, so treatment of silicosis is aimed at slowing down the disease and relieving its symptoms.
In 1995, the World Health Organization called for the elimination of silicosis by 2030, but research studies and news stories show it remains a threat to many workers.
Below, we have gathered several studies on the topic to help journalists bolster their reporting with academic research.
Research roundup
Artificial Stone Associated Silicosis: A Systematic Review
Veruscka Leso, et al. International Journal of Environmental Research and Public Health, February 2019.This systematic review aims to verify the association between exposure to silica dust in artificial stone and the development of silicosis.
Researchers narrowed down their selection from 75 papers to seven studies that met their inclusion criteria. The seven studies were from Australia, Israel and Spain. Most of the studies are observational and impede a definite association between exposure to silica while working with artificial stone and developing silicosis, the authors note.
However, “the unusually high incidence of the disease that was reported over short periods of investigations, and the comparable occupational histories of affected workers, all being involved in the manufacture and manipulation of engineered stones, may indicate a cause-effect relationship of this type.”
The review of studies reveals a lack of basic preventive measures such as lack of access to disposable masks; lack of information and training on the dangers of silica dust; and lack of periodic medical examinations, including a chest X-ray, among workers. There was limited environmental monitoring of dust levels at the workplace. Also, there was no dust suppression system, such as the use of water when polishing the stones, or effective ventilation. Machinery and tools weren’t properly set up and didn’t undergo routine checks, the authors write.
The authors recommend environmental monitoring for assessing silica levels in the workplace and verifying the effectiveness of personal protections. They also recommend the health surveillance of workers exposed to silica dust.
“Stakeholders, manufacturers, occupational risk prevention services, insurance companies for occupational accidents and diseases, business owners, occupational health physicians, general practitioners, and also employees should be engaged, not only in designing/planning processes and operational working environments, but also in assessing the global applicability of proactive preventive and protective measures to identify and control crystalline silica exposure, especially in new and unexpected exposure scenarios, the full extent of which cannot yet be accurately predicted,” they write.
Silica-Related Diseases in the Modern World
Ryan F. Hoy and Daniel C. Chambers. Allergy, November 2020.The study is a review of the mineralogy of silica, epidemiology, clinical and radiological features of the various forms of silicosis and other diseases associated with exposure to silica.
The primary factor associated with the development of silicosis is the intensity and duration of cumulative exposure to silica dust. Most countries regulate silica dust occupational exposure limits, generally in the range of 0.05 mg/m3 to 0.1 mg/m3, although the risk of dust exposure to workers still remains high at those levels.
The study provides a list of activities that could expose workers to silica dust. They include abrasive blasting of sand and sandstone; cement and brick manufacturing; mixing, glazing or sculpting of china, ceramic and pottery; construction involving bricklaying, concrete cutting, paving and demolition; sandblasting denim jeans; working with and polishing dental materials; mining and related milling; handling raw material during paint manufacturing; road and highway construction and repair; soap and cosmetic production; blasting and drilling tunnels; and waste incineration.
“Despite the large number of workers in the construction sector, there have been few studies of [silica dust] exposure in this industry,” the authors note.
Other than silicosis, conditions associated with silica exposure include sarcoidosis, an inflammatory disease that commonly affects the lungs and lymph nodes, autoimmune disease, lung cancer and pulmonary infections.
“Recent outbreaks of silica-associated disease highlight the need for constant vigilance to identify and control new and well-established sources of silica exposure. While there are currently no effective treatments for silicosis, it is a completely preventable lung disease,” the authors write.
A Systematic Review of the Effectiveness of Dust Control Measures Adopted to Reduce Workplace Exposure
Frederick Anlimah, Vinod Gopaldasani, Catherine MacPhail and Brian Davies. Environmental Science and Pollution Research International, March 2023.This study provides an overview of various interventions and their effectiveness in preventing exposure to silica dust based on a review of 133 studies from 16 countries, including the U.S., Canada, China, India, Taiwan and Australia, and published between 2010 and 2020.
These dust control measures range from simple work practices such as the use of respirators to more sophisticated technologies, such as water and air curtains and foam technology, the authors note.
The review finds increasing research interest in dust reduction, mainly in China. But overall, regulatory influence remains inadequate in preventing miners’ exposure to silica dust.
“Results from the review suggest that adopted interventions increase knowledge, awareness, and attitudes about respirator usage and generate positive perceptions about respirator usage while reducing misconceptions,” the authors write. “Interventions can increase the use, proper use, and frequency of use of respirators and the adoption readiness for dust controls but may not provide sustained motivation in workers for the continual use of dust controls or [personal protective equipment.]”
Notes from the Field: Surveillance of Silicosis Using Electronic Case Reporting — California, December 2022–July 2023
Jennifer Flattery, et al. Morbidity and Mortality Weekly Report, November 2023.This study examines the use of electronic case reporting to identify silicosis cases in California. Electronic case reporting, or eCR, is the automated, real-time exchange of case report information between electronic health records at health facilities at state and local public health agencies in the U.S. It is a joint effort between the Association of Public Health Laboratories, the Council of State and Territorial Epidemiologists, and the CDC. Currently, 208 health conditions can be reported using eCR. All 50 states and other U.S.-affiliated jurisdictions are connected to eCR. Once a public health agency receives a case report, it reaches out to the patient for contact tracing or other actions.
From October 2022 to July 2023, the California Department of Public Health received initial silicosis case reports for 41 individuals. A review of medical records confirmed 19 cases and 16 probable cases. Six of the 41 cases were considered unlikely to be silicosis after a review of medical records.
Notably, engineered stone countertop fabrication was a significant source of exposure, especially among Hispanic and Latino workers.
At least seven of the 19 confirmed cases were associated with the fabrication of engineered stone — quartz — countertops. The 19 patients’ ages ranged from 33 to 51 and all were Hispanic or Latino. One patient died and two had both lungs replaced. One was evaluated for a lung transplant.
The median age of the 35 patients with probable or confirmed silicosis was 65, ranging from 33 to 89 years, and 91% were men.
“It is important that health care providers routinely ask patients about their work as an important determinant of health,” the authors write. “Being aware of the risks associated with work exposures, as well as the regulations, medical monitoring, and prevention strategies that address those risks can help guide patient care.”
Additional research
Understanding the Pathogenesis of Engineered Stone-Associated Silicosis: The Effect of Particle Chemistry on the Lung Cell Response
Chandnee Ramkissoon, et al. Respirology, December 2023.Silicosis, Tuberculosis and Silica Exposure Among Artisanal and Small-Scale Miners: A Systematic Review and Modelling Paper
Patrick Howlett, et al. PLOS Global Public Health, September 2023.Silicosis Among Immigrant Engineered Stone (Quartz) Countertop Fabrication Workers in California
Jane C. Fazio, et al. JAMA Internal Medicine, July 2023.Silicosis and Tuberculosis: A Systematic Review and Meta-Analysis
P. Jamshidi, et al. Pulmonology, June 2023.From Basic Research to Clinical Practice: Considerations for Treatment Drugs for Silicosis
Rou Li, Huimin Kang and Shi Chen. International Journal of Molecular Science, May 2023.Silicosis After Short-Term Exposure
J. Nowak-Pasternak, A. Lipińska-Ojrzanowska and B. Świątkowska. Occupational Medicine, January 2023.Occupational Silica Exposure and Dose-Response for Related Disorders—Silicosis, Pulmonary TB, AIDs and Renal Diseases: Results of a 15-Year Israeli Surveillance
Rachel Raanan, et al. International Journal of Environmental Research and Public Health, November 2022.Demographic, Exposure and Clinical Characteristics in a Multinational Registry of Engineered Stone Workers with Silicosis
Jeremy Tang Hua, et al. Occupational & Environmental Medicine, August 2022.Current Global Perspectives on Silicosis — Convergence of Old and Newly Emergent Hazards
Ryan F. Hoy, et al. Respirology, March 2022.The Association Between Silica Exposure, Silicosis and Tuberculosis: A systematic Review and Metal-Analysis
Rodney Ehrlich, Paula Akugizibwe, Nandi Siegfried and David Rees. BMC Public Health, May 2021.Silicosis, Progressive Massive Fibrosis and Silico-Tuberculosis Among Workers with Occupational Exposure to Silica Dusts in Sandstone Mines of Rajasthan State
Subroto Nandi, Sarang Dhatrak, Kamalesh Sarkar. Journal of Family Medicine and Primary Care, February 2021.Artificial Stone Silicosis: Rapid Progression Following Exposure Cessation
Antonio León-Jiménez, et al. Chest, September 2020.Silica-Associated Lung Disease: An Old-World Exposure in Modern Industries
Hayley Barnes, Nicole S.L. Goh, Tracy L. Leong and Ryan Hoy. Respirology, September 2019.Australia Reports on Audit of Silicosis for Stonecutters
Tony Kirby. The Lancet, March 2019.Artificial Stone-Associated Silicosis: A Rapidly Emerging Occupational Lung Disease
Ryan F. Hoy, et al. Occupational & Environmental Medicine, December 2017.This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: