Life Extension Multivitamins vs Centrum Multivitamins – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Life Extension Multivitamins to Centrum Multivitamins, we picked the Life Extension.
Why?
The clue here was on the label: “two per day”. It’s not so that they can sell extra filler! It’s because they couldn’t fit it all into one.
While the Centrum Multivitamins is a (respectably) run-of-the-mill multivitamin (and multimineral) containing reasonable quantities of most vitamins and minerals that people supplement, the Life Extension product has the same plus more:
- More of the vitamins and minerals; i.e. more of them are hitting 100%+ of the RDA
- More beneficial supplements, including:
- Inositol, Alpha lipoic acid, Bio-Quercetin phytosome, phosphatidylcholine complex, Marigold extract, Apigenin, Lycopene, and more that we won’t list here because it starts to get complicated if we do.
We’ll have to write some main features on some of those that we haven’t written about before, but suffice it to say, they’re all good things.
Main take-away for today: sometimes more is better; it just necessitates then reading the label to check.
Want to get some Life Extension Multivitamins (and/or perhaps just read the label on the back)? Here they are on Amazon
PS: it bears mentioning, since we are sometimes running brands against each other head-to-head in this section: nothing you see here is an advertisement/sponsor unless it’s clearly marked as such. We haven’t, for example, been paid by Life Extension or any agent of theirs, to write the above. It’s just our own research and conclusion.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
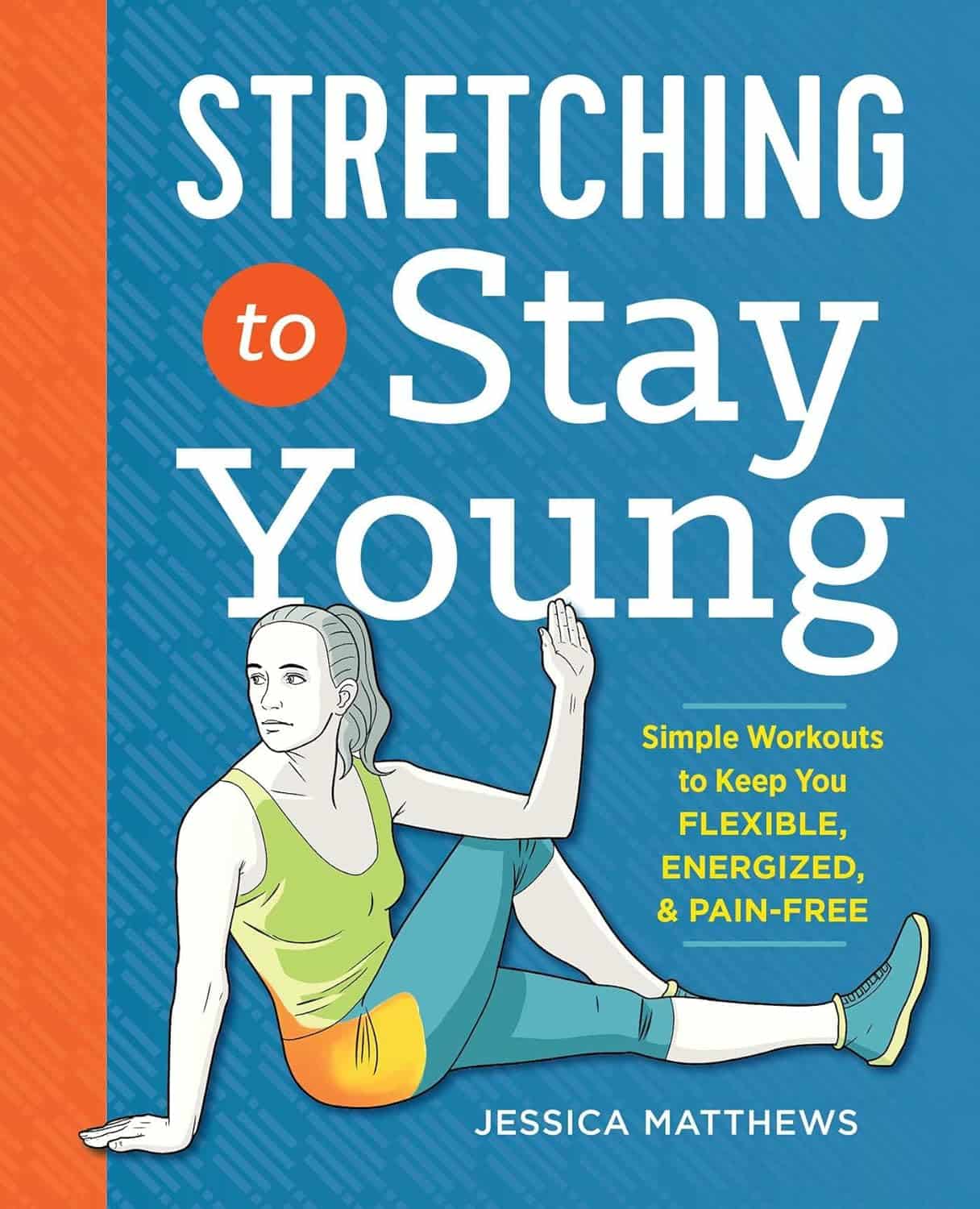
Stretching to Stay Young – by Jessica Matthews
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of stretching gurus (especially the Instagrammable kind) offer advices like “if you can’t do the splits balanced between two chairs to start with, that’s fine… just practise by doing the splits against a wall first!”
Jessica Matthews, meanwhile, takes a more grounded approach. A lot of this is less like yoga and more like physiotherapy—it’s uncomplicated and functional. There’s nothing flashy here… just the promise of being able to thrive in your body; supple and comfortable, doing the activities that matter to you.
On which note: the book gives advices about stretches for before and after common activities, for example:
- a bedtime routine set
- a pre-gardening set
- a post-phonecall set
- a level-up-your golf set
- a get ready for dancing set
…and many more. Whether “your thing” is cross-country skiing or knitting, she’s got you covered.
The book covers the whole body from head to toe. Whether you want to be sure to stretch everything, or just work on a particular part of your body that needs special attention, it’s there… with beautifully clear illustrations (the front cover illustration is indicative of the style—note how the muscle being stretched is highlighted in orange, too) and simple, easy-to-understand instructions.
All in all, we’re none of us getting any younger, but we sure can take some of our youth into whatever years come next. This is the stuff that life is made of!
Get your copy of “Stretching To Stay Young” from Amazon today!
Share This Post
-
Chipotle Chili Wild Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a very gut-healthy recipe that’s also tasty and filling, and packed with polyphenols too. What’s not to love?
You will need
- 1 cup cooked wild rice (we suggest cooking it with 1 tbsp chia seeds added)
- 7 oz cooked sweetcorn (can be from a tin or from frozen or cook it yourself)
- 4 oz charred jarred red peppers (these actually benefit from being from a jar—you can use fresh or frozen if necessary, but only jarred will give you the extra gut-healthy benefits from fermentation)
- 1 avocado, pitted, peeled, and cut into small chunks
- ½ red onion, thinly sliced
- 6–8 sun-dried tomatoes, chopped
- 2 tbsp extra virgin olive oil
- 2 tsp chipotle chili paste (adjust per your heat preferences)
- 1 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of 1 lime
Method
(we suggest you read everything at least once before doing anything)
1) Mix the cooked rice, red onion, sweetcorn, red peppers, avocado pieces, and sun-dried tomato, in a bowl. We recommend to do it gently, or you will end up with guacamole in there.
2) Mix the olive oil, lime juice, chipotle chili paste, black pepper, and MSG/salt, in another bowl. If perchance you have a conveniently small whisk, now is the time to use it. Failing that, a fork will suffice.
3) Add the contents of the second bowl to the first, tossing gently but thoroughly to combine well, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brown Rice vs Wild Rice – Which is Healthier?
- Making Friends With Your Gut (You Can Thank Us Later)
- Capsaicin For Weight Loss And Against Inflammation
Take care!
Share This Post
-
Why Zebras Don’t Get Ulcers – by Dr. Robert M. Sapolsky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book does kick off with a section that didn’t age well—he talks of the stress induced globally by the Spanish Flu pandemic of 1918, and how that kind of thing just doesn’t happen any more. Today, we have much less existentially dangerous stressors!
However, the fact we went and had another pandemic really only adds weight to the general arguments of the book, rather than detracting.
We are consistently beset by “the slings and arrows of outrageous fortune” as Shakespeare would put it, and there’s a reason (or twenty) why many people go grocery-shopping with the cortisol levels of someone being hunted for sport.
So, why don’t zebras get ulcers, as they actually are hunted for food?
They don’t have rent to pay or a mortgage, they don’t have taxes, or traffic, or a broken washing machine, or a project due in the morning. Their problems come one at a time. They have a useful stress response to a stressful situation (say, being chased by lions), and when the danger is over, they go back to grazing. They have time to recover.
For us, we are (usually) not being chased by lions. But we have everything else, constantly, around the clock. So, how to fix that?
Dr. Sapolsky comprehensively describes our physiological responses to stress in quite different terms than many. By reframing stress responses as part of the homeostatic system—trying to get the body back into balance—we find a solution, or rather: ways to help our bodies recover.
The style is “pop-science” and is very accessible for the lay reader while still clearly coming from a top-level academic who is neck-deep in neuroendocrinological research. Best of both worlds!
Bottom line: if you try to take very day at a time, but sometimes several days gang up on you at once, and you’d like to learn more about what happens inside you as a result and how to fix that, this book is for you!
Click here to check out “Why Zebras Don’t Get Ulcers” and give yourself a break!
Share This Post
Related Posts
-
The Four Pillar Plan – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rangan Chatterjee, a medical doctor, felt frustrated with how many doctors in his field focus on treating the symptoms of disease, rather than the cause. Sometimes, of course, treating the symptom is necessary too! But neglecting the cause is a recipe for long-term woes.
What he does differently is take lifestyle as a foundation, and even that, he does differently than many authors on the topic. How so, you may wonder?
Rather than look first at exercise and diet, he starts with “relax”. His rationale is reasonable: diving straight in with marathon training or a whole new diet plan can be unsustainable without this as a foundation to fall back on.
Many sources look first at exercise (because it can be a very simple “prescription”) before diet (often more complex)… but how does one exercise well with the wrong fuel in the tank? So Dr. Chatterjee’s titular “Four Pillars” come in the following order:
- Relax
- Eat
- Move
- Sleep
He also goes for “move” rather than “exercise” as the focus here is more on minimizing time spent sitting, and thus involving a lot of much more frequent gentle activities… rather than intensive training programs and the like.
And as for sleep? Yes, that comes last because—no matter how important it is—the other things are easier to directly control. After all, one can improve conditions for sleep, but one cannot simply choose to sleep better! So with the other three things covered first, good sleep is the fourth and final thing to fall into place.
All in all, this is a great book to cut through the catch-22 problem of lifestyle factors negatively impacting each other.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Edam vs Gouda – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edam to gouda, we picked the edam.
Why?
There’s not a lot between them, but there are some differences:
In terms of macros, their numbers are all close enough that one may beat the other by decimal place rounding, so we’ll call this a tie. Same goes for their fat type breakdowns; per 100g they both have 18g saturated, 8g monounsaturated, and 1g polyunsaturated.
In the category of vitamins, edam has slightly more of vitamins A, B1, B2, and B3, while gouda has slightly more of vitamins B5 and B9. A modest 4:2 win for edam.
When it comes to minerals, edam has more calcium, iron, and potassium, while gouda is not higher in any minerals. A more convincing win for edam.
In short, enjoy either or both in moderation, but if you’re going to choose one over the other, edam is the way to go.
Want to learn more?
You might like to read:
Can Saturated Fats Be Healthy?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: