‘I keep away from people’ – combined vision and hearing loss is isolating more and more older Australians
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our ageing population brings a growing crisis: people over 65 are at greater risk of dual sensory impairment (also known as “deafblindness” or combined vision and hearing loss).
Some 66% of people over 60 have hearing loss and 33% of older Australians have low vision. Estimates suggest more than a quarter of Australians over 80 are living with dual sensory impairment.
Combined vision and hearing loss describes any degree of sight and hearing loss, so neither sense can compensate for the other. Dual sensory impairment can occur at any point in life but is increasingly common as people get older.
The experience can make older people feel isolated and unable to participate in important conversations, including about their health.

Causes and conditions
Conditions related to hearing and vision impairment often increase as we age – but many of these changes are subtle.
Hearing loss can start as early as our 50s and often accompany other age-related visual changes, such as age-related macular degeneration.
Other age-related conditions are frequently prioritised by patients, doctors or carers, such as diabetes or heart disease. Vision and hearing changes can be easy to overlook or accept as a normal aspect of ageing. As an older person we interviewed for our research told us
I don’t see too good or hear too well. It’s just part of old age.
An invisible disability
Dual sensory impairment has a significant and negative impact in all aspects of a person’s life. It reduces access to information, mobility and orientation, impacts social activities and communication, making it difficult for older adults to manage.
It is underdiagnosed, underrecognised and sometimes misattributed (for example, to cognitive impairment or decline). However, there is also growing evidence of links between dementia and dual sensory loss. If left untreated or without appropriate support, dual sensory impairment diminishes the capacity of older people to live independently, feel happy and be safe.
A dearth of specific resources to educate and support older Australians with their dual sensory impairment means when older people do raise the issue, their GP or health professional may not understand its significance or where to refer them. One older person told us:
There’s another thing too about the GP, the sort of mentality ‘well what do you expect? You’re 95.’ Hearing and vision loss in old age is not seen as a disability, it’s seen as something else.
Isolated yet more dependent on others
Global trends show a worrying conundrum. Older people with dual sensory impairment become more socially isolated, which impacts their mental health and wellbeing. At the same time they can become increasingly dependent on other people to help them navigate and manage day-to-day activities with limited sight and hearing.
One aspect of this is how effectively they can comprehend and communicate in a health-care setting. Recent research shows doctors and nurses in hospitals aren’t making themselves understood to most of their patients with dual sensory impairment. Good communication in the health context is about more than just “knowing what is going on”, researchers note. It facilitates:
- shorter hospital stays
- fewer re-admissions
- reduced emergency room visits
- better treatment adherence and medical follow up
- less unnecessary diagnostic testing
- improved health-care outcomes.
‘Too hard’
Globally, there is a better understanding of how important it is to maintain active social lives as people age. But this is difficult for older adults with dual sensory loss. One person told us
I don’t particularly want to mix with people. Too hard, because they can’t understand. I can no longer now walk into that room, see nothing, find my seat and not recognise [or hear] people.
Again, these experiences increase reliance on family. But caring in this context is tough and largely hidden. Family members describe being the “eyes and ears” for their loved one. It’s a 24/7 role which can bring frustration, social isolation and depression for carers too. One spouse told us:
He doesn’t talk anymore much, because he doesn’t know whether [people are] talking to him, unless they use his name, he’s unaware they’re speaking to him, so he might ignore people and so on. And in the end, I noticed people weren’t even bothering him to talk, so now I refuse to go. Because I don’t think it’s fair.

So, what can we do?
Dual sensory impairment is a growing problem with potentially devastating impacts.
It should be considered a unique and distinct disability in all relevant protections and policies. This includes the right to dedicated diagnosis and support, accessibility provisions and specialised skill development for health and social professionals and carers.
We need to develop resources to help people with dual sensory impairment and their families and carers understand the condition, what it means and how everyone can be supported. This could include communication adaptation, such as social haptics (communicating using touch) and specialised support for older adults to navigate health care.
Increasing awareness and understanding of dual sensory impairment will also help those impacted with everyday engagement with the world around them – rather than the isolation many feel now.
Moira Dunsmore, Senior Lecturer, Sydney Nursing School, Faculty of Medicine and Health, University of Sydney, University of Sydney; Annmaree Watharow, Lived Experience Research Fellow, Centre for Disability Research and Policy, University of Sydney, and Emily Kecman, Postdoctoral research fellow, Department of Linguistics, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pain Clinics Made Millions From ‘Unnecessary’ Injections Into ‘Human Pin Cushions’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McMINNVILLE, Tenn. — Each month, Michelle Shaw went to a pain clinic to get the shots that made her back feel worse — so she could get the pills that made her back feel better.
Shaw, 56, who has been dependent on opioid painkillers since she injured her back in a fall a decade ago, said in both an interview with KFF Health News and in sworn courtroom testimony that the Tennessee clinic would write the prescriptions only if she first agreed to receive three or four “very painful” injections of another medicine along her spine.
The clinic claimed the injections were steroids that would relieve her pain, Shaw said, but with each shot her agony would grow. Shaw said she eventually tried to decline the shots, then the clinic issued an ultimatum: Take the injections or get her painkillers somewhere else.
“I had nowhere else to go at the time,” Shaw testified, according to a federal court transcript. “I was stuck.”
Shaw was among thousands of patients of Pain MD, a multistate pain management company that was once among the nation’s most prolific users of what it referred to as “tendon origin injections,” which normally inject a single dose of steroids to relieve stiff or painful joints. As many doctors were scaling back their use of prescription painkillers due to the opioid crisis, Pain MD paired opioids with monthly injections into patients’ backs, claiming the shots could ease pain and potentially lessen reliance on painkillers, according to federal court documents.
Now, years later, Pain MD’s injections have been proved in court to be part of a decade-long fraud scheme that made millions by capitalizing on patients’ dependence on opioids. The Department of Justice has successfully argued at trial that Pain MD’s “unnecessary and expensive injections” were largely ineffective because they targeted the wrong body part, contained short-lived numbing medications but no steroids, and appeared to be based on test shots given to cadavers — people who felt neither pain nor relief because they were dead.
Four Pain MD employees have pleaded guilty or been convicted of health care fraud, including company president Michael Kestner, who was found guilty of 13 felonies at an October trial in Nashville, Tennessee. According to a transcript from Kestner’s trial that became public in December, witnesses testified that the company documented giving patients about 700,000 total injections over about eight years and said some patients got as many as 24 shots at once.
“The defendant, Michael Kestner, found out about an injection that could be billed a lot and paid well,” said federal prosecutor James V. Hayes as the trial began, according to the transcript. “And they turned some patients into human pin cushions.”
The Department of Justice declined to comment for this article. Kestner’s attorneys either declined to comment or did not respond to requests for an interview. At trial, Kestner’s attorneys argued that he was a well-intentioned businessman who wanted to run pain clinics that offered more than just pills. He is scheduled to be sentenced on April 21 in a federal court in Nashville.
According to the transcript of Kestner’s trial, Shaw and three other former patients testified that Pain MD’s injections did not ease their pain and sometimes made it worse. The patients said they tolerated the shots only so Pain MD wouldn’t cut off their prescriptions, without which they might have spiraled into withdrawal.
“They told me that if I didn’t take the shots — because I said they didn’t help — I would not get my medication,” testified Patricia McNeil, a former patient in Tennessee, according to the trial transcript. “I took the shots to get my medication.”
In her interview with KFF Health News, Shaw said that often she would arrive at the Pain MD clinic walking with a cane but would leave in a wheelchair because the injections left her in too much pain to walk.
“That was the pain clinic that was supposed to be helping me,” Shaw said in her interview. “I would come home crying. It just felt like they were using me.”
‘Not Actually Injections Into Tendons at All’
Pain MD, which sometimes operated under the name Mid-South Pain Management, ran as many as 20 clinics in Tennessee, Virginia, and North Carolina throughout much of the 2010s. Some clinics averaged more than 12 injections per patient each month, and at least two patients each received more than 500 shots in total, according to federal court documents.
All those injections added up. According to Medicare data filed in federal court, Pain MD and Mid-South Pain Management billed Medicare for more than 290,000 “tendon origin injections” from January 2010 to May 2018, which is about seven times that of any other Medicare biller in the U.S. over the same period.
Tens of thousands of additional injections were billed to Medicaid and Tricare during those same years, according to federal court documents. Pain MD billed these government programs for about $111 per injection and collected more than $5 million from the government for the shots, according to the court documents.
More injections were billed to private insurance too. Christy Wallace, an audit manager for BlueCross BlueShield of Tennessee, testified that Pain MD billed the insurance company about $40 million for more than 380,000 injections from January 2010 to March 2013. BlueCross paid out about $7 million before it cut off Pain MD, Wallace said.
These kinds of enormous billing allegations are not uncommon in health care fraud cases, in which fraudsters sometimes find a legitimate treatment that insurance will pay for and then overuse it to the point of absurdity, said Don Cochran, a former U.S. attorney for the Middle District of Tennessee.
Tennessee alone has seen fraud allegations for unnecessary billing of urine testing, skin creams, and other injections in just the past decade. Federal authorities have also investigated an alleged fraud scheme involving a Tennessee company and hundreds of thousands of catheters billed to Medicare, according to The Washington Post, citing anonymous sources.
Cochran said the Pain MD case felt especially “nefarious” because it used opioids to make patients play along.
“A scheme where you get Medicare or Medicaid money to provide a medically unnecessary treatment is always going to be out there,” Cochran said. “The opioid piece just gives you a universe of compliant people who are not going to question what you are doing.”
“It was only opioids that made those folks come back,” he said.
The allegations against Pain MD became public in 2018 when Cochran and the Department of Justice filed a civil lawsuit against the company, Kestner, and several associated clinics, alleging that Pain MD defrauded taxpayers and government insurance programs by billing for “tendon origin injections” that were “not actually injections into tendons at all.”
Kestner, Pain MD, and several associated clinics have each denied all allegations in that lawsuit, which is ongoing.Scott Kreiner, an expert on spine care and pain medicine who testified at Kestner’s criminal trial, said that true tendon origin injections (or TOIs) typically are used to treat inflamed joints, like the condition known as “tennis elbow,” by injecting steroids or platelet-rich plasma into a tendon. Kreiner said most patients need only one shot at a time, according to the transcript.
But Pain MD made repeated injections into patients’ backs that contained only lidocaine or Marcaine, which are anesthetic medications that cause numbness for mere hours, Kreiner testified. Pain MD also used needles that were often too short to reach back tendons, Kreiner said, and there was no imaging technology used to aim the needle anyway. Kreiner said he didn’t find any injections in Pain MD’s records that appeared medically necessary, and even if they had been, no one could need so many.
“I simply cannot fathom a scenario where the sheer quantity of TOIs that I observed in the patient records would ever be medically necessary,” Kreiner said, according to the trial transcript. “This is not even a close call.”
Jonathan White, a physician assistant who administered injections at Pain MD and trained other employees to do so, then later testified against Kestner as part of a plea deal, said at trial that he believed Pain MD’s injection technique was based on a “cadaveric investigation.”
According to the trial transcript, White said that while working at Pain MD he realized he could find no medical research that supported performing tendon origin injections on patients’ backs instead of their joints. When he asked if Pain MD had any such research, White said, an employee responded with a two-paragraph letter from a Tennessee anatomy professor — not a medical doctor — that said it was possible to reach the region of back tendons in a cadaver by injecting “within two fingerbreadths” of the spine. This process was “exactly the procedure” that was taught at Pain MD, White said.
During his own testimony, Kreiner said it was “potentially dangerous” to inject a patient as described in the letter, which should not have been used to justify medical care.
“This was done on a dead person,” Kreiner said, according to the trial transcript. “So the letter says nothing about how effective the treatment is.”
Over-Injecting ‘Killed My Hand’
Pain MD collapsed into bankruptcy in 2019, leaving some patients unable to get new prescriptions because their medical records were stuck in locked storage units, according to federal court records.
At the time, Pain MD defended the injections and its practice of discharging patients who declined the shots. When a former patient publicly accused the company of treating his back “like a dartboard,” Pain MD filed a defamation lawsuit, then dropped the suit about a month later.
“These are interventional clinics, so that’s what they offer,” Jay Bowen, a then-attorney for Pain MD, told The Tennessean newspaper in 2019. “If you don’t want to consider acupuncture, don’t go to an acupuncture clinic. If you don’t want to buy shoes, don’t go to a shoe store.”
Kestner’s trial told another story. According to the trial transcript, eight former Pain MD medical providers testified that the driving force behind Pain MD’s injections was Kestner himself, who is not a medical professional and yet regularly pressured employees to give more shots.
One nurse practitioner testified that she received emails “every single workday” pushing for more injections. Others said Kestner openly ranked employees by their injection rates, and implied that those who ranked low might be fired.
“He told me that if I had to feed my family based on my productivity, that they would starve,” testified Amanda Fryer, a nurse practitioner who was not charged with any crime.
Brian Richey, a former Pain MD nurse practitioner who at times led the company’s injection rankings, and has since taken a plea deal that required him to testify in court, said at the trial that he “performed so many injections” that his hand became chronically inflamed and required surgery.
“‘Over injecting killed my hand,’” Richey said on the witness stand, reading a text message he sent to another Pain MD employee in 2017, according to the trial transcript. “‘I was in so much pain Injecting people that didnt want it but took it to stay a patient.’”
“Why would they want to stay there?” a prosecutor asked.
“To keep getting their narcotics,” Richey responded, according to the trial transcript.
Throughout the trial, defense attorney Peter Strianse argued that Pain MD’s focus on injections was a result of Kestner’s “obsession” with ensuring that the company “would never be called a pill mill.”
Strianse said that Kestner “stayed up at night worrying” about patients coming to clinics only to get opioid prescriptions, so he pushed his employees to administer injections, too.
“Employers motivating employees is not a crime,” Strianse said at closing arguments, according to the court transcript. “We get pushed every day to perform. It’s not fraud; it’s a fact of life.”
Prosecutors insisted that this defense rang hollow. During the trial, former employees had testified that most patients’ opioid dosages remained steady or increased while at Pain MD, and that the clinics did not taper off the painkillers no matter how many injections were given.
“Giving them injections does not fix the pill mill problem,” federal prosecutor Katherine Payerle said during closing arguments, according to the trial transcript. “The way to fix being a pill mill is to stop giving the drugs or taper the drugs.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Thinner Leaner Stronger – by Michael Matthews
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, the elephant in the training room: this book does assume that you want to be thinner, leaner, and stronger. This is the companion book, written for women, to “Bigger, Stronger, Leaner”, which was written for men. Statistically, these assumptions are reasonable, even if the generalizations are imperfect. Also, this reviewer has a gripe with anything selling “thinner”. Leaner was already sufficient, and “stronger” is the key element here, so “thinner” is just marketing, and marketing something that’s often not unhealthy, to sell a book that’s actually full of good advice for building a healthy body.
In other words: don’t judge a book by the cover, however eyeroll-worthy it may be.
The book is broadly aimed at middle-aged readers, but boasts equal worth for young and old alike. If there’s something Matthews knows how to do well in his writing, it’s hedging his bets.
As for what’s in the book: it’s diet and exercise advice, aimed at long-term implementation (i.e. not a crash course, but a lifestyle change), for maximum body composition change results while not doing anything silly (like many extreme short-term courses do) and not compromising other aspects of one’s health, while also not taking up an inordinate amount of time.
The dietary advice is sensible, broadly consistent with what we’d advise here, and/but if you want to maximise your body composition change results, you’re going to need a pocket calculator (or be better than this writer is at mental arithmetic).
The exercise advice is detailed, and a lot more specific than “lift things”; there are programs of specifically how many sets and reps and so forth, and when to increase the weights and when not to.
A strength of this book is that it explains why all those numbers are what they are, instead of just expecting the reader to take on faith that the best for a given exercise is (for example) 3 sets of 8–10 reps of 70–75% of one’s single-rep max for that exercise. Because without the explanation, those numbers would seem very arbitrary indeed, and that wouldn’t help anyone stick with the program. And so on, for any advice he gives.
The style is… A little flashy for this reader’s taste, a little salesy (and yes he does try to upsell to his personal coaching, but really, anything you need is in the book already), but when it comes down to it, all that gym-boy bravado doesn’t take away from the fact his advice is sound and helpful.
Bottom line: if you would like your body to be the three things mentioned in the title, this book can certainly help you get there.
Click here to check out Thinner Leaner Stronger, and become thinner, leaner, stronger!
Share This Post
-
Finding Peace at the End of Life – by Henry Fersko-Weiss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not the most cheery book we’ve reviewed, but it is an important one. From its first chapter, with “a tale of two deaths”, one that went as well as can be reasonably expected, and the other one not so much, it presents a lot of choices.
The book is not prescriptive in its advice regarding how to deal with these choices, but rather, investigative. It’s thought-provoking, and asks questions—tacitly and overtly.
While the subtitle says “for families and caregivers”, it’s as much worth when it comes to managing one’s own mortality, too, by the way.
As for the scope of the book, it covers everything from terminal diagnosis, through the last part of life, to the death itself, to all that goes on shortly afterwards.
Stylewise, it’s… We’d call it “easy-reading” for style, but obviously the content is very heavy, so you might want to read it a bit at a time anyway, depending on how sensitive to such topics you are.
Bottom line: this book is not exactly a fun read, but it’s a very worthwhile one, and a good way to avoid regrets later.
Share This Post
Related Posts
-
The Comfort Book – by Matt Haig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book “is what it says on the tin”. Matt Haig, bestselling author of “Reasons to Stay Alive” (amongst other works) is here with “a hug in a book”.
The format of the book is an “open it at any page and you’ll find something of value” book. Its small chapters are sometimes a few pages long, but often just a page. Sometimes just a line. Always deep.
All of us, who live long enough, will ponder our mortality sometimes. The feelings we may have might vary on a range from “afraid of dying” to “despairing of living”… but Haig’s single biggest message is that life is full of wonder; each moment precious.
- That hope is an incredible (and renewable!) resource.
- That we are more than a bad week, or month, or year, or decade.
- That when things are taken from us, the things that remain have more value.
Bottom line: you might cry (this reviewer did!), but it’ll make your life the richer for it, and remind you—if ever you need it—the value of your amazing life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
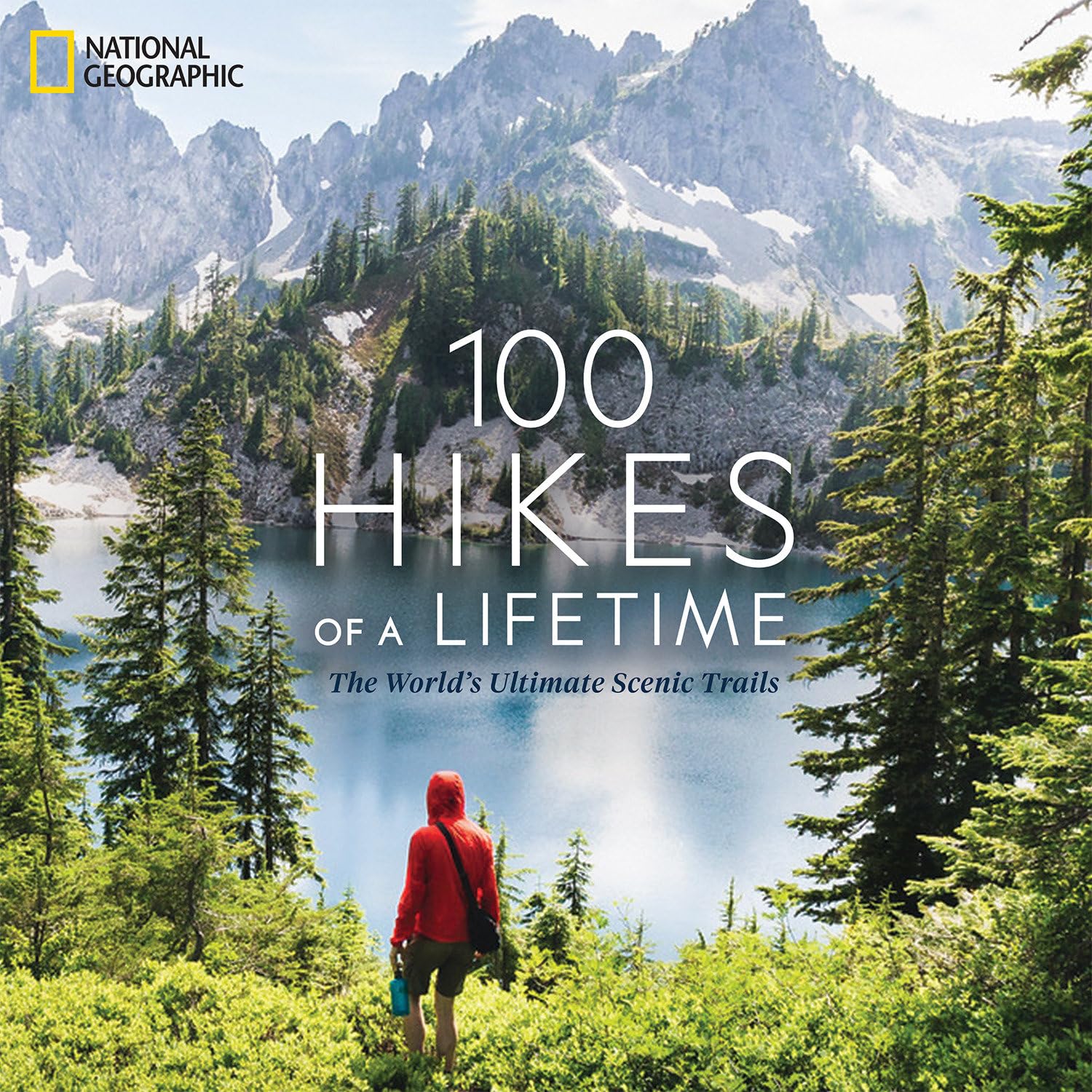
100 Hikes of a Lifetime – by Kate Siber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is published by National Geographic, so you can imagine the quality of the photos throughout.
Inside, and after a general introduction and guide to gear and packing appropriately, it’s divided into continents, with a diverse array of “trips of a lifetime” for anyone who enjoys hiking.
It’s not a narrative book, rather, it is a guide, a little in the style of “Lonely Planet”, with many “know before you go” tips, information about the best time to go, difficult level, alternative routes if you want to get most of the enjoyment while having an easier time of it (or, conversely, if you want to see some extra sights along the way), and what to expect at all points.
Where the book really excels is in balancing inspiration with information. There are some books that make you imagine being in a place, but you’ll never actually go there. There are other books that are technical manuals but not very encouraging. This one does both; it provides the motivation and the “yes, you really can, here’s how” information that, between them, can actually get you packing and on your way.
Bottom line: if you yearn for breathtaking views and time in the great outdoors, but aren’t sure where to start, this will give you an incredible menu to choose from, and give you the tools to go about doing it.
Click here to check out 100 Hikes Of A Lifetime, and live it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is cold water bad for you? The facts behind 5 water myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know the importance of staying hydrated, especially in hot weather. But even for something as simple as a drink of water, conflicting advice and urban myths abound.
Is cold water really bad for your health? What about hot water from the tap? And what is “raw water”? Let’s dive in and find out.
Myth 1: Cold water is bad for you
Some recent TikToks have suggested cold water causes health problems by somehow “contracting blood vessels” and “restricting digestion”. There is little evidence for this.
While a 2001 study found 51 out of 669 women tested (7.6%) got a headache after drinking cold water, most of them already suffered from migraines and the work hasn’t been repeated since.
Cold drinks were shown to cause discomfort in people with achalasia (a rare swallowing disorder) in 2012 but the study only had 12 participants.
For most people, the temperature you drink your water is down to personal preference and circumstances. Cold water after exercise in summer or hot water to relax in winter won’t make any difference to your overall health.
Myth 2: You shouldn’t drink hot tap water
This belief has a grain of scientific truth behind it. Hot water is generally a better solvent than cold water, so may dissolve metals and minerals from pipes better. Hot water is also often stored in tanks and may be heated and cooled many times. Bacteria and other disease-causing microorganisms tend to grow better in warm water and can build up over time.
It’s better to fill your cup from the cold tap and get hot water for drinks from the kettle.
Myth 3: Bottled water is better
While bottled water might be safer in certain parts of the world due to pollution of source water, there is no real advantage to drinking bottled water in Australia and similar countries.
According to University of Queensland researchers, bottled water is not safer than tap water. It may even be tap water. Most people can’t tell the difference either. Bottled water usually costs (substantially) more than turning on the tap and is worse for the environment.
What about lead in tap water? This problem hit the headlines after a public health emergency in Flint, Michigan, in the United States. But Flint used lead pipes with a corrosion inhibitor (in this case orthophosphate) to keep lead from dissolving. Then the city switched water sources to one without a corrosion inhibitor. Lead levels rose and a public emergency was declared.
Fortunately, lead pipes haven’t been used in Australia since the 1930s. While lead might be present in some old plumbing products, it is unlikely to cause problems.
Myth 4: Raw water is naturally healthier
Some people bypass bottled and tap water, going straight to the source.
The “raw water” trend emerged a few years ago, encouraging people to drink from rivers, streams and lakes. There is even a website to help you find a local source.
Supporters say our ancestors drank spring water, so we should, too. However, our ancestors also often died from dysentery and cholera and their life expectancy was low.
While it is true even highly treated drinking water can contain low levels of things like microplastics, unless you live somewhere very remote, the risks of drinking untreated water are far higher as it is more likely to contain pollutants from the surrounding area.
Myth 5: It’s OK to drink directly from hoses
Tempting as it may be, it’s probably best not to drink from the hose when watering the plants. Water might have sat in there, in the warm sun for weeks or more potentially leading to bacterial buildup.
Similarly, while drinking water fountains are generally perfectly safe to use, they can contain a variety of bacteria. It’s useful (though not essential) to run them for a few seconds before you start to drink so as to get fresh water through the system rather than what might have been sat there for a while.
We are fortunate to be able to take safe drinking water for granted. Billions of people around the world are not so lucky.
So whether you like it hot or cold, or somewhere in between, feel free to enjoy a glass of water this summer.
Just don’t drink it from the hose.
Oliver A.H. Jones, Professor of chemistry, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: