Garlic vs Ginger – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing garlic to ginger, we picked the ginger.
Why?
Both are great, and it is close!
Notwithstanding that (almost?) nobody eats garlic or ginger for the macros, let’s do a moment’s due diligence on that first: garlic has more than 3x the protein and about 2x the fiber (and slightly higher carbs). But, given the small quantities in which people usually consume these foods, these numbers aren’t too meaningful.
In the category of micronutrients, garlic has a lot more vitamins and minerals. We’ll not do a full breakdown for this though, because again, unless you’re eating it by the cupful, this won’t make a huge difference.
Which means that so far, we have two nominal wins for garlic.
Both plants have many medicinal properties. They are both cardioprotective and anticancer, and both full of antioxidants. The benefits of both are comparable in these regards.
Both have antidiabetic action also, but ginger’s effects are stronger when compared head-to head.
So that’s an actual practical win for ginger.
Each plant’s respective effects on the gastrointestinal tract sets them further apart—ginger has antiemetic effects and can be used for treating nausea and vomiting from a variety of causes. Garlic, meanwhile, can cause adverse gastrointestinal effects in some people—but it’s usually neutral for most people in this regard.
Another win for ginger in practical terms.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Matters Most For Your Heart?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat More (Of This) For Lower Blood Pressure
Heart disease remains the world’s #1 killer. We’d say “and in the US, it’s no different”, but in fact, the US is #1 country for heart disease. So, it’s worse and perhaps some extra care is in order.
But how?
What matters the most
Is it salt? Salt plays a part, but it’s not even close to the top problem:
Hypertension: Factors Far More Relevant Than Salt
Is it saturated fat? Saturated fat from certain sources plays more of a role than salt, but other sources may not be so much of an issue:
Can Saturated Fats Be Heart-Healthy?
Is it red meat? Red meat is not great for the heart (or for almost anything else, except perhaps anemia):
The Whys and Hows of Cutting Meats Out Of Your Diet
…but it’s still not the top dietary factor.
The thing many don’t eat
All the above are foodstuffs that a person wanting a healthier heart and cardiovascular system in general might (reasonably and usually correctly) want to cut down, but there’s one thing that most people need more of:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
And this is especially true for heart health:
❝Dietary fiber has emerged as a crucial yet underappreciated part of hypertension management.
Our comprehensive analysis emphasizes the evidence supporting the effectiveness of dietary fiber in lowering blood pressure and reducing the risk of cardiovascular events.❞
Specifically, she and her team found:
- Each additional 5g of fiber per day reduces blood pressure by 2.8/2.1 (systolic/diastolic, in mmHG)
- Dietary fiber works in several ways to improve cardiovascular health, including via gut bacteria, improved lipids profiles, and anti-inflammatory effects
- Most people are still only getting a small fraction (¼ to ⅓) of the recommended daily amount of fiber. To realize how bad that is, imagine if you consumed only ¼ of the recommended daily amount of calories every day!
You can read more about it here:
Dietary fiber critical in managing hypertension, international study finds
That’s a pop-science article, but it’s still very informative. If you prefer to read the scientific paper itself (or perhaps as well), you can find it below
Recommendations for the Use of Dietary Fiber to Improve Blood Pressure Control
Want more from your fiber?
Here’s yet another way fiber improves cardiometabolic health, hot off the academic press (the study was published just a couple of weeks ago):
How might fiber lower diabetes risk? Your gut could hold the clues
this pop-science article was based on this scientific paper
Gut Microbiota and Blood Metabolites Related to Fiber Intake and Type 2 Diabetes
Take care!
Share This Post
-
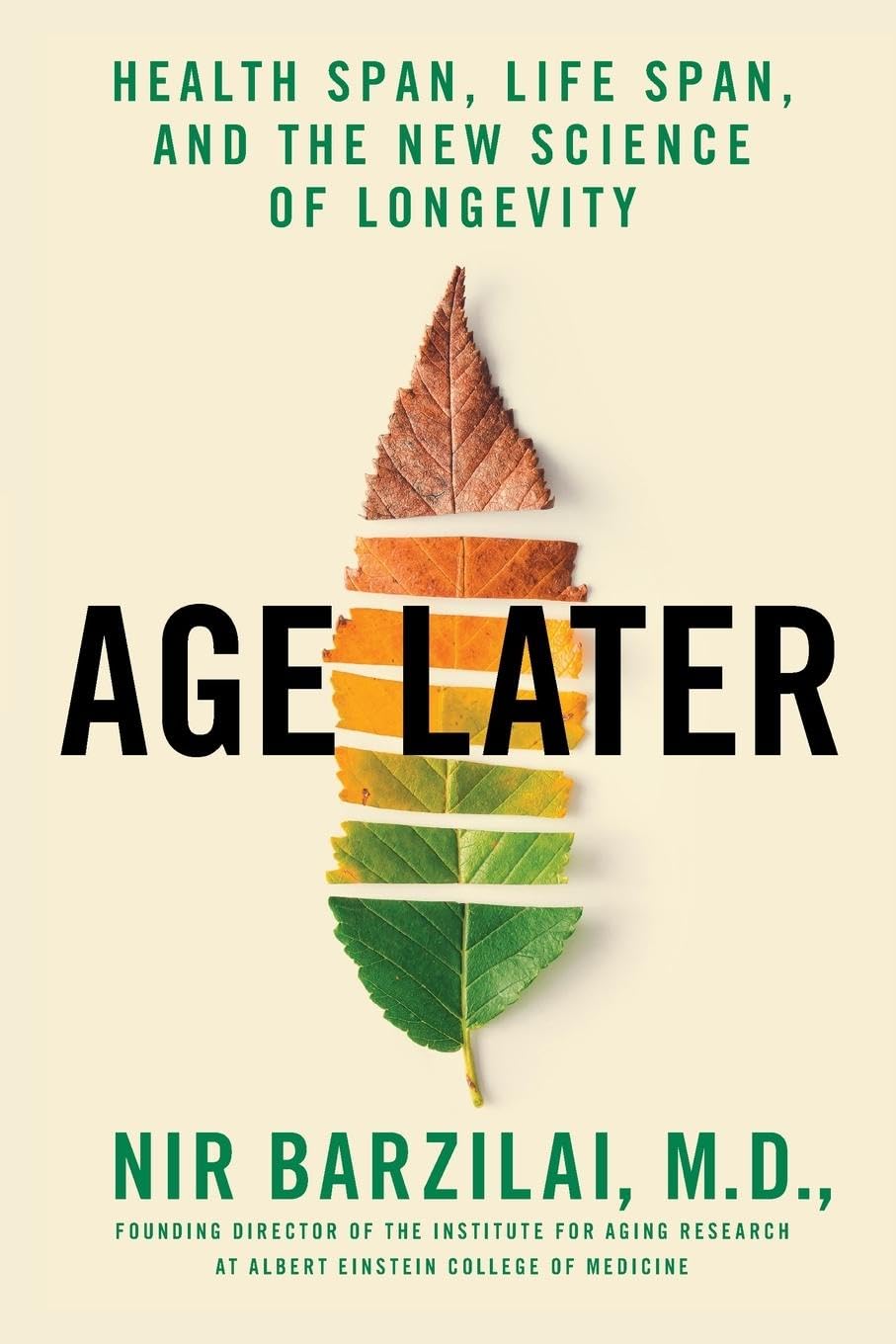
Age Later – by Dr. Nir Barzilai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Barzilai discusses why we age, why supercentenarians age more slowly, and even, why it is so often the case that supercentenarians outside of Blue Zones have poor lifestyles (their longevity is because of protective genes that mitigate the harmful effects of those poor lifestyles—the ultimate in “survivorship bias”).
He also talks not just genetics, but also epigenetics, and thus gene expression. Bearing in mind, there’s a scale of modifiability there: with current tech, we can’t easily change a bad gene… But we often can just switch it off (or at least downregulate its expression). This is where studies in supercentenarians are helpful even for those who don’t have such fortunate genes—the supercentenarian studies show us which genes we want on or off, what gene expressions to aim for, etc. Further clinical studies can then show us what lifestyle interventions (exercise, diet, nutraceuticals, etc) can do that for us.
With regard to those lifestyle interventions, he does cover many, and that’s where a lot of the practical value of the book comes from. But it’s not just “do this, do that”; understanding the reasons behind why things work the way they do is important, so as to be more likely to do it right, and also to enjoy greater adherence (we tend to do things we understand more readily than things we have just been told to do).
There are areas definitely within the author’s blind spots—for example, when talking about menopausal HRT, he discusses at great length the results of the discredited WHI study, and considers it the only study of relevance. So, this is a reminder to not believe everything said by someone who sounds confident (Dr. Barzilai’s professional background is mostly in treating diabetes).
In terms of style, it is very much narrative; somewhat pop-science, but more “this doctor wants to tell stories”. So many stories. Now, the stories all have informational value, so this isn’t padding, but it is the style, so we mention it as such. As for citations, there aren’t any, so if you want to look up the science he mentions, you’re going to need a bit of digital sleuthery to find the papers from the clues in the stories.
Bottom line: if you’re interested in the science of aging and how that has been progressing for the past decades and where we’re at, this book will give you so many jumping-off points, and is an engaging read.
Share This Post
-
Kate Middleton is having ‘preventive chemotherapy’ for cancer. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, is undergoing treatment for cancer. In a video thanking followers for their messages of support after her major abdominal surgery, the Princess of Wales explained, “tests after the operation found cancer had been present.”
“My medical team therefore advised that I should undergo a course of preventative chemotherapy and I am now in the early stages of that treatment,” she said in the two-minute video.
No further details have been released about the Princess of Wales’ treatment.
But many have been asking what preventive chemotherapy is and how effective it can be. Here’s what we know about this type of treatment.
It’s not the same as preventing cancer
To prevent cancer developing, lifestyle changes such as diet, exercise and sun protection are recommended.
Tamoxifen, a hormone therapy drug can be used to reduce the risk of cancer for some patients at high risk of breast cancer.
Aspirin can also be used for those at high risk of bowel and other cancers.
How can chemotherapy be used as preventive therapy?
In terms of treating cancer, prevention refers to giving chemotherapy after the cancer has been removed, to prevent the cancer from returning.
If a cancer is localised (limited to a certain part of the body) with no evidence on scans of it spreading to distant sites, local treatments such as surgery or radiotherapy can remove all of the cancer.
If, however, cancer is first detected after it has spread to distant parts of the body at diagnosis, clinicians use treatments such as chemotherapy (anti-cancer drugs), hormones or immunotherapy, which circulate around the body .
The other use for chemotherapy is to add it before or after surgery or radiotherapy, to prevent the primary cancer coming back. The surgery may have cured the cancer. However, in some cases, undetectable microscopic cells may have spread into the bloodstream to distant sites. This will result in the cancer returning, months or years later.
With some cancers, treatment with chemotherapy, given before or after the local surgery or radiotherapy, can kill those cells and prevent the cancer coming back.
If we can’t see these cells, how do we know that giving additional chemotherapy to prevent recurrence is effective? We’ve learnt this from clinical trials. Researchers have compared patients who had surgery only with those whose surgery was followed by additional (or often called adjuvant) chemotherapy. The additional therapy resulted in patients not relapsing and surviving longer.
How effective is preventive therapy?
The effectiveness of preventive therapy depends on the type of cancer and the type of chemotherapy.
Let’s consider the common example of bowel cancer, which is at high risk of returning after surgery because of its size or spread to local lymph glands. The first chemotherapy tested improved survival by 15%. With more intense chemotherapy, the chance of surviving six years is approaching 80%.
Preventive chemotherapy is usually given for three to six months.
How does chemotherapy work?
Many of the chemotherapy drugs stop cancer cells dividing by disrupting the DNA (genetic material) in the centre of the cells. To improve efficacy, drugs which work at different sites in the cell are given in combinations.
Chemotherapy is not selective for cancer cells. It kills any dividing cells.
But cancers consist of a higher proportion of dividing cells than the normal body cells. A greater proportion of the cancer is killed with each course of chemotherapy.
Normal cells can recover between courses, which are usually given three to four weeks apart.
What are the side effects?
The side effects of chemotherapy are usually reversible and are seen in parts of the body where there is normally a high turnover of cells.
The production of blood cells, for example, is temporarily disrupted. When your white blood cell count is low, there is an increased risk of infection.
Cell death in the lining of the gut leads to mouth ulcers, nausea and vomiting and bowel disturbance.
Certain drugs sometimes given during chemotherapy can attack other organs, such as causing numbness in the hands and feet.
There are also generalised symptoms such as fatigue.
Given that preventive chemotherapy given after surgery starts when there is no evidence of any cancer remaining after local surgery, patients can usually resume normal activities within weeks of completing the courses of chemotherapy.
Ian Olver, Adjunct Professsor, School of Psychology, Faculty of Health and Medical Sciences, University of Adelaide
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
4 ways to cut down on meat when dining out – and still make healthy choices
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us are looking for ways to eat a healthier and more sustainable diet. And one way to do this is by reducing the amount of meat we eat.
That doesn’t mean you need to become a vegan or vegetarian. Our recent research shows even small changes to cut down on meat consumption could help improve health and wellbeing.
But not all plant-based options are created equal and some are ultra-processed. Navigating what’s available when eating out – including options like tofu and fake meats – can be a challenge.
So what are your best options at a cafe or restaurant? Here are some guiding principles to keep in mind when cutting down on meat.
Mikhaylovskiy/Shutterstock Health benefits to cutting down
Small amounts of lean meat can be part of a healthy, balanced diet. But the majority of Australians still eat more meat than recommended.
Only a small percentage of Australians (10%) are vegetarian or vegan. But an increasing number opt for a flexitarian diet. Flexitarians eat a diet rich in fruits and vegetables, while still enjoying small amounts of meat, dairy, eggs and fish.
Our recent research looked at whether the average Australian diet would improve if we swapped meat and dairy for plant-based alternatives, and the results were promising.
The study found health benefits when people halved the amount of meat and dairy they ate and replaced them with healthy plant-based foods, like tofu or legumes. On average, their dietary fibre intake – which helps with feeling fuller for longer and digestive health – went up. Saturated fats – which increase our blood cholesterol levels, a risk factor for heart disease – went down.
Including more fibre and less saturated fat helps reduce the risk of heart disease.
Achieving these health benefits may be as simple as swapping ham for baked beans in a toastie for lunch, or substituting half of the mince in your bolognese for lentils at dinner.
Filling your plate with fibre-rich foods can help lower cholesterol. Wally Pruss/Shutterstock How it’s made matters
For a long time we’ve known processed meats – such as ham, bacon and sausages – are bad for your health. Eating high amounts of these foods is associated with poor heart health and some forms of cancer.
But the same can be true of many processed meat alternatives.
Plant-based alternatives designed to mimic meat, such as sausages and burgers, have become readily available in supermarkets, cafes and restaurants. These products are ultra-processed and can be high in salt and saturated fat.
Our study found when people replaced meat and dairy with ultra-processed meat alternatives – such as plant-based burgers or sausages – they ate more salt and less calcium, compared to eating meat or healthy plant-based options.
So if you’re cutting down on meat for health reasons, it’s important to think about what you’re replacing it with. The Australian Dietary Guidelines recommend eggs, legumes/beans, tofu, nuts and seeds.
Tofu can be a great option. But we recommend flavouring plain tofu with herbs and spices yourself, as pre-marinated products are often ultra-processed and can be high in salt.
What about when dining out?
When you’re making your own food, it’s easier to adapt recipes or reduce the amount of meat. But when faced with a menu, it can be difficult to work out what is the best option.
Eating a range of colours is one way to ensure variety. Mikhail Nilov/Pexels Here are our four ways to make healthy choices when you eat out:
1. Fill half your plate with vegetables
When cutting down on meat, aim for half your plate to be vegetables. Try to also eat a variety of colours, such as leafy green spinach, red capsicum and pumpkin.
When you’re out, this might look like choosing a vegetable-based entree, a stir-fry or ordering a side salad to have with your meal.
2. Avoid the deep fryer
The Australian Dietary Guidelines recommend limiting deep fried foods to once a week or less. When dining out, choose plant-based options that are sautéed, grilled, baked, steamed, boiled or poached – instead of those that are crumbed or battered before deep frying.
This could mean choosing vegetarian dumplings that are steamed not fried, or poached eggs at brunch instead of fried. Ordering a side of roast vegetables instead of hot chips is also a great option.
3. Pick wholegrains
Scan the menu for wholegrain options such as brown rice, wholemeal pizza or pasta, barley, quinoa or wholemeal burger buns. Not only are they good sources of protein, but they also provide more dietary fibre than refined grains, which help keep you fuller for longer.
4. If you do pick meat – choose less processed kinds
You may not always want, or be able, to make a vegetarian choice when eating out and with other people. If you do opt for meat, it’s better to steer clear of processed options like bacon or sausages.
If sharing dishes with other people, you could try adding unprocessed plant-based options into the mix. For example, a curry with lentils or chickpeas, or a vegetable-based pizza instead of one with ham or salami. If that’s not an option, try choose meat that’s a lean cut, such as chicken breast, or options which are grilled rather than fried.
Laura Marchese, PhD candidate at the Institute for Physical Activity and Nutrition, Deakin University and Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Navigating the health-care system is not easy, but you’re not alone.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hello, dear reader!
This is my first column for Healthy Debate as a Patient Navigator. This column will be devoted to providing patients with information to help them through their journey with the health-care system and answering your questions.
Here’s a bit about me: I have been a patient partner at The Ottawa Hospital and Ottawa Hospital Research Institute since 2017, and have joined a variety of governance boards that work on patient and caregiver engagement such as the Patient Advisors Network, the Ontario Health East Region Patient and Family Advisory Council and the Equity in Health Systems Lab.
My journey as a patient partner started much before 2017 though. When I was a teenager, I was diagnosed with a cholesteatoma, a rare and chronic disease that causes the development of fatty tumors in the middle ear. I have had multiple surgeries to try to fix it but will need regular follow-ups to monitor whether the tumor returns. Because of this, I also live with an invisible disability since I have essentially become functionally deaf in one ear and often rely on a hearing aid when I navigate the world.
Having undergone three surgeries in my adolescent years, it was my experience undergoing surgery for an acute hand and wrist injury following a jet ski accident as an adult that was the catalyst for my decision to become a patient partner. There was an intriguing contrast between how I was cared for at two different health-care institutions, my age being the deciding factor at which hospital I went to (a children’s hospital or an adult one).
The most memorable example was how, as a teenager or child, you were never left alone before surgery, and nurses and staff took all the time necessary to comfort me and answer my (and my family’s) questions. I also remember how right before putting me to sleep, the whole staff initiated a surgical pause and introduced themselves and explained to me what their role was during my surgery.
None of that happened as an adult. I was left in a hallway while the operating theater was prepared, anxious and alone with staff walking by not even batting an eye. My questions felt like an annoyance to the care team; as soon as I was wheeled onto the operating room table, the anesthetist quickly put me to sleep. I didn’t even have the time to see who else was there.
Now don’t get me wrong: I am incredibly appreciative with the quality of care I received, but it was the everyday interactions with the care teams that I felt could be improved. And so, while I was recovering from that surgery, I looked for a way to help other patients and the hospital improve its care. I discovered the hospital’s patient engagement program, applied, and the rest is history!
Since then, I have worked on a host of patient-centered policy and research projects and fervently advocate that surgical teams adopt a more compassionate approach with patients before and after surgery.
I’d be happy to talk a bit more about my journey if you ask, but with that out of the way … Welcome to our first patient navigator column about patient engagement.
Conceptualizing the continuum of Patient Engagement
In the context of Canadian health care, patient engagement is a multifaceted concept that involves active collaboration between patients, caregivers, health-care providers and researchers. It involves patients and caregivers as active contributors in decision-making processes, health-care services and medical research. Though the concept is not new, the paradigm shift toward patient engagement in Canada started around 2010.
I like to conceptualize the different levels of patient engagement as a measure of the strength of the relationship between patients and their interlocutors – whether it’s a healthcare provider, administrator or researcher – charted against the duration of the engagement or the scope of input required from the patient.
Defining different levels of Patient Engagement
Following the continuum, let’s begin by defining different levels of patient engagement. Bear in mind that these definitions can vary from one organization to another but are useful in generally labelling the level of patient engagement a project has achieved (or wishes to achieve).
Patient involvement: If the strength of the relationship between patients and their interlocutors is minimal and not time consuming or too onerous, then perhaps it can be categorized as patient involvement. This applies to many instances of transactional engagement.
Patient advisory/consulting: Right in the middle of our continuum, patients can find themselves engaging in patient advisory or consulting work, where projects are limited in scope and duration or complexity, and the relationship is not as profound as a partnership.
Patient partnership: The stronger the relationship is between the patient and their interlocutor, and the longer the engagement activity lasts or how much input the patient is providing, the more this situation can be categorized as patient partnership. It is the inverse of patient involvement.
Examples of the different levels of Patient Engagement
Let’s pretend you are accompanying a loved one to an appointment to manage a kidney disease, requiring them to undergo dialysis treatment. We’ll use this scenario to exemplify what label could be used to describe the level of engagement.
Patient involvement: In our case, if your loved one – or you – fills out a satisfaction or feedback survey about your experience in the waiting room and all that needed to be done was to hand it back to the clerk or care team, then, at a basic level, you could likely label this interaction as a form of patient involvement. It can also involve open consultations around a design of a new look and feel for a hospital, or the understandability of a survey or communications product. Interactions with the care team, administrators or researchers are minimal and often transactional.
Patient advisory/consulting: If your loved one was asked for more detailed information about survey results over the course of a few meetings, this could represent patient advisory/consulting. This could mean that patients meet with program administrators and care providers and share their insights on how things can be improved. It essentially involves patients providing advice to health-care institutions from the perspective of patients, their family members and caregivers.
Patient advisors or consultants are often appointed by hospitals or academic institutions to offer insights at multiple stages of health-care delivery and research. They can help pilot an initiative based on that feedback or evaluate whether the new solutions are working. Often patient advisors are engaged in smaller-term individual projects and meet with the project team as regularly as required.
Patient partnership: Going above and beyond patient advisory, if patients have built a trusting relationship with their care team or administrators, they could feel comfortable enough to partner with them and initiate a project of their own. This could be for a project in which they study a different form of treatment to improve patient-centered outcomes (like the time it takes to feel “normal” following a session); it could be working together to identify and remove barriers for other patients that need to access that type of care. These projects are not fulfilled overnight, but require a collaborative, longstanding and trusting relationship between patients and health-care providers, administrators or researchers. It ensures that patients, regardless of severity or chronicity of their illness, can meaningfully contribute their experiences to aid in improving patient care, or develop or implement policies, pilots or research projects from start to finish.
It is leveraging that lived and living experience to its full extent and having the patient partner involved as an equal voice in the decision-making process for a project – over many months, usually – that the engagement could be labeled a partnership.
Last words
The point of this column will be to answer or explore issues or questions related to patient engagement, health communications or even provide some thoughts on how to handle a particular situation.
I would be happy to collect your questions and feedback at any time, which will help inform future columns. Just email me at [email protected] or connect with me on social media (Linked In, X / Twitter).
It’s not easy to navigate our health-care systems, but you are not alone.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Grow New Brain Cells (At Any Age)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Grow New Brain Cells (At Any Age)
It was long believed that brain growth could not occur later in life, due to expending our innate stock of pluripotent stem cells. However, this was mostly based on rodent studies.
Rodent studies are often used for brain research, because it’s difficult to find human volunteers willing to have their brains sliced thinly (so that the cells can be viewed under a microscope) at the end of the study.
However, neurobiologist Dr. Maura Boldrini led a team that did a lot of research by means of autopsies on the hippocampi of (previously) healthy individuals ranging in age from 14 to 79.
What she found is that while indeed the younger subjects did predictably have more young brain cells (neural progenitors and immature neurons), even the oldest subject, at the age of 79, had been producing new brain cells up until death.
Read her landmark study: Human Hippocampal Neurogenesis Persists throughout Aging
There was briefly a flurry of news articles about a study by Dr. Shawn Sorrels that refuted this, however, it later came to light that Dr. Sorrels had accidentally destroyed his own evidence during the cell-fixing process—these things happen; it’s just unfortunate the mistake was not picked up until after publication.
A later study by a Dr. Elena Moreno-Jiménez fixed this flaw by using a shorter fixation time for the cell samples they wanted to look at, and found that there were tens of thousands of newly-made brain cells in samples from adults ranging from 43 to 87.
Now, there was still a difference: the samples from the youngest adult had 30% more newly-made braincells than the 87-year-old, but given that previous science thought brain cell generation stopped in childhood, the fact that an 87-year-old was generating new brain cells 30% less quickly than a 43-year-old is hardly much of a criticism!
As an aside: samples from patients with Alzheimer’s also had a 30% reduction in new braincell generation, compared to samples from patients of the same age without Alzheimer’s. But again… Even patients with Alzheimer’s were still growing some new brain cells.
Read it for yourself: Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease
Practical advice based on this information
Since we can do neurogenesis at any age, but the rate does drop with age (and drops sharply in the case of Alzheimer’s disease), we need to:
Feed your brain. The brain is the most calorie-consuming organ we have, by far, and it’s also made mostly of fat* and water. So, get plenty of healthy fats, and get plenty of water.
*Fun fact: while depictions in fiction (and/or chemically preserved brains) may lead many to believe the brain has a rubbery consistency, the untreated brain being made of mostly fat and water gives it more of a blancmange-like consistency in reality. That thing is delicate and spatters easily. There’s a reason it’s kept cushioned inside the strongest structure of our body, far more protected than anything in our torso.
Exercise. Specifically, exercise that gets your blood pumping. This (as our earlier-featured video today referenced) is one of the biggest things we can do to boost Brain-Derived Neurotrophic Factor, or BDNF.
Here be science: Brain-Derived Neurotrophic Factor, Depression, and Physical Activity: Making the Neuroplastic Connection
However, that’s not the only way to increase BDNF; another is to enjoy a diet rich in polyphenols. These can be found in, for example, berries, tea, coffee, and chocolate. Technically those last two are also botanically berries, but given how we usually consume them, and given how rich they are in polyphenols, they merit a special mention.
See for example: Effects of nutritional interventions on BDNF concentrations in humans: a systematic review
Some supplements can help neuron (re)growth too, so if you haven’t already, you might want to check out our previous main feature on lion’s mane mushroom, a supplement which does exactly that.
For those who like videos, you may also enjoy this TED talk by neuroscientist Dr. Sandrine Thuret:
Prefer text? Click here to read the transcript
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: