Fiber Fueled – by Dr. Will Bulsiewicz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We generally know that for gut health we should eat fiber, but what of the balances of different sorts of fiber?
That’s one of the main things that make this book stand out—fostering diversity in our microbiome by fostering diversity in our diet. Specifically, diversity of fiber-containing foods.
The book is part “science made easy for the lay reader”, and part recipe book. The recipes come with shopping lists and a meal planner, though we would recommend to use those as a guide rather than to try to adhere perfectly to them.
In particular, this reviewer would encourage much more generous use of healthful seasonings… and less reliance on there being leftovers several days later (tasty food gets gone quickly in this house!)
As for the science, the feel of this is more like reading a science-based observational documentary with explanations, than of reading a science textbook. Studies are mentioned in passing, but not dissected in any detail, and the focus is more on getting the key learnings across.
Bottom line: if you’d like to boost not just the amount, but also the diversity, of fiber in your diet, and reap the gut-health rewards, this book is a great guide for that!
Click here to get your copy of “Fiber Fueled” from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Drug Metabolism (When You’re Not Average!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Your Medications Run Out… Of You
Everybody knows that alcohol can affect medications’ effects, but what of smoking, and what of obesity? And how does the alcohol thing work anyway?
It’s all about the enzymes
Medicines that are processed by the liver (which is: most medicines) are metabolized there by specialist enzymes, and the things we do can increase or decrease the quantity of those enzymes—and/or how active they are.
Dr. Kata Wolff Pederson and her team of researchers at Aarhus University in Denmark examined the livers of recently deceased donors in ways that can’t (ethically) be done with live patients, and were able to find the associations between various lifestyle factors and different levels of enzymes responsible for drug metabolism.
And it’s not always how you might think!
Some key things they found:
- Smokers have twice as high levels of enzyme CYP1A2 than non-smokers, which results in the faster metabolism of a lot of drugs.
- Drinkers have 30% higher levels of enzyme CYP2E1, which also results in a faster metabolism of a lot of drugs.
- Patients with obesity have 50% lower levels of enzyme CYP3A4, resulting in slower metabolism of many drugs
This gets particularly relevant when we take into account the next fact:
- Of the individuals in the study, 40% died from poisoning from a mixture of drugs (usually: prescription and otherwise)
Read in full: Sex- and Lifestyle-Related Factors are Associated with Altered Hepatic CYP Protein Levels
Read a pop-sci article about it: Your lifestyle can determine how well your medicine will work
How much does the metabolism speed matter?
It can matter a lot! If you’re taking drugs and carefully abiding by the dosage instructions, those instructions were assuming they know your speed of metabolism, and this is based on an average.
- If your metabolism is faster, you can get too much of a drug too quickly, and it can harm you
- If your metabolism is faster, it also means that while yes it’ll start working sooner, it’ll also stop working sooner
- If it’s a painkiller, that’s inconvenient. If it’s a drug that keeps you alive, then well, that’s especially unfortunate.
- If your metabolism is slower, it can mean your body is still processing the previous dose(s) when you take the next one, and you can overdose (and potentially die)
We touched on this previously when we talked about obesity in health care settings, and how people can end up getting worse care:
As for alcohol and drugs? Obviously we do not recommend, but here’s some of the science of it with many examples:
Why it’s a bad idea to mix alcohol with some medications
Take care!
Share This Post
-
When the Body Says No – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know that chronic stress is bad for us because of what it does to our cortisol levels, so what is the rest of this book about?
Dr. Gabor Maté is a medical doctor, heavily specialized in the impact of psychological trauma on long term physical health.
Here, he examies—as the subtitle promises—the connection between stress and disease. As it turns out, it’s not that simple.
We learn not just about the impact that stress has on our immune system (including increasing the risk of autoimmune disorders like rheumatoid arthritis), the cardiovascular system, and various other critical systems fo the body… But also:
- how environmental factors and destructive coping styles contribute to the onset of disease, and
- how traumatic events can warp people’s physical perception of pain
- how certain illnesses are associated with particular personality types.
This latter is not “astrology for doctors”, by the way. It has more to do with what coping strategies people are likely to employ, and thus what diseases become more likely to take hold.
The book has practical advice too, and it’s not just “reduce your stress”. Ideally, of course, indeed reduce your stress. But that’s a) obvious b) not always possible. Rather, Dr. Maté explains which coping strategies result in the least prevalence of disease.
In terms of writing style, the book is very much easy-reading, but be warned that (ironically) this isn’t exactly a feel-good book. There are lot of tragic stories in it. But, even those are very much well-worth reading.
Bottom line: if you (and/or a loved one) are suffering from stress, this book will give you the knowledge and understanding to minimize the harm that it will otherwise do.
Click here to check out When The Body Says No, and take good care of yourself; you’re important!
Share This Post
-
Toxic Gas That Sterilizes Medical Devices Prompts Safety Rule Update
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, Madeline Beal has heard frustration and even bewilderment during public meetings about ethylene oxide, a cancer-causing gas that is used to sterilize half of the medical devices in the U.S.
Beal, senior risk communication adviser for the Environmental Protection Agency, has fielded questions about why the agency took so long to alert people who live near facilities that emit the chemical about unusually high amounts of the carcinogenic gas in their neighborhoods. Residents asked why the EPA couldn’t close those facilities, and they wanted to know how many people had developed cancer from their exposure.
“If you’re upset by the information you’re hearing tonight, if you’re angry, if it scares you to think about risk to your family, those are totally reasonable responses,” Beal told an audience in Laredo, Texas, in September 2022. “We think the risk levels near this facility are too high.”
There are about 90 sterilizing plants in the U.S. that use ethylene oxide, and for decades companies used the chemical to sterilize medical products without drawing much attention. Many medical device-makers send their products to the plants to be sterilized before they are shipped, typically to medical distribution companies.
But people living around these facilities have been jolted in recent years by a succession of warnings about cancer risk from the federal government and media reports, an awareness that has also spawned protests and lawsuits alleging medical harm.
The EPA is expected to meet a March 1 court-ordered deadline to finalize tighter safety rules around how the toxic gas is used. The proposed changes come in the wake of a 2016 agency report that found that long-term exposure to ethylene oxide is more dangerous than was previously thought.
But the anticipated final rules — the agency’s first regulatory update on ethylene oxide emissions in more than a decade — are expected to face pushback. Medical device-makers worry stricter regulation will increase costs and may put patients at higher risk of infection from devices, ranging from surgical kits to catheters, due to deficient sterilization. The new rules are also not likely to satisfy the concerns of environmentalists or members of the public, who already have expressed frustration about how long it took the federal government to sound the alarm.
“We have been breathing this air for 40 years,” said Connie Waller, 70, who lives with her husband, David, 75, within two miles of such a sterilizing plant in Covington, Georgia, east of Atlanta. “The only way to stop these chemicals is to hit them in their pocketbook, to get their attention.”
The EPA says data shows that long-term exposure to ethylene oxide can increase the risk of breast cancer and cancers of the white blood cells, such as non-Hodgkin lymphoma, myeloma, and lymphocytic leukemia. It can irritate the eyes, nose, throat, and lungs, and has been linked to damage to the brain and nervous and reproductive systems. Children are potentially more vulnerable, as are workers routinely exposed to the chemical, EPA officials say. The agency calculates the risk based on how much of the gas is in the air or near the sterilizing facility, the distance a person is from the plant, and how long the person is exposed.
Waller said she was diagnosed with breast cancer in 2004 and that her husband was found to have non-Hodgkin lymphoma eight years later.
A 2022 study of communities living near a sterilization facility in Laredo found the rates of acute lymphocytic leukemia and breast cancer were greater than expected based on statewide rates, a difference that was statistically significant.
Beal, the EPA risk adviser, who regularly meets with community members, acknowledges the public’s concerns. “We don’t think it’s OK for you to be at increased risk from something that you have no control over, that’s near your house,” she said. “We are working as fast as we can to get that risk reduced with the powers that we have available to us.”
In the meantime, local and state governments and industry groups have scrambled to defuse public outcry.
Hundreds of personal injury cases have been filed in communities near sterilizing plants. In 2020, New Mexico’s then-attorney general filed a lawsuit against a plant in Santa Teresa, and that case is ongoing. In a case that settled last year in suburban Atlanta, a company agreed to pay $35 million to 79 people who alleged ethylene oxide used at the plant caused cancer and other injuries.
In Cook County, Illinois, a jury in 2022 awarded $363 million to a woman who alleged exposure to ethylene oxide gas led to her breast cancer diagnosis. But, in another Illinois case, a jury ruled that the sterilizing company was not liable for a woman’s blood cancer claim.
Greg Crist, chief advocacy officer for the Advanced Medical Technology Association, a medical device trade group that says ethylene oxide is an effective and reliable sterilant, attributes the spate of lawsuits to the litigious nature of trial attorneys.
“If they smell blood in the water, they’ll go after it,” Crist said.
Most states have at least one sterilizing plant. According to the EPA, a handful, like California and North Carolina, have gone further than the agency and the federal Clean Air Act to regulate ethylene oxide emissions. After a media and political firestorm raised awareness about the metro Atlanta facilities, Georgia started requiring sterilizing plants that use the gas to report all leaks.
The proposed rules the EPA is set to finalize would set lower emissions limits for chemical plants and commercial sterilizers and increase some safety requirements for workers within these facilities. The agency is expected to set an 18-month deadline for commercial sterilizers to come into compliance with the emissions rules.
That would help at facilities that “cut corners,” with lax pollution controls that allow emissions of the gas into nearby communities, said Richard Peltier, a professor of environmental health sciences at the University of Massachusetts-Amherst. Stronger regulation also prevents the plants from remaining under the radar. “One of the dirty secrets is that a lot of it is self-regulated or self-policed,” Peltier added.
But the proposed rules did not include protections for workers at off-site warehouses that store sterilized products, which can continue to emit ethylene oxide. They also did not require air testing around the facilities, prompting debate about how effective they would be in protecting the health of nearby residents.
Industry officials also don’t expect an alternative that is as broadly effective as ethylene oxide to be developed anytime soon, though they support researching other methods. Current alternatives include steam, radiation, and hydrogen peroxide vapor.
Increasing the use of alternatives can reduce industry dependence on “the crutch of ethylene oxide,” said Darya Minovi, senior analyst with the Union of Concerned Scientists, an advocacy group.
But meeting the new guidelines will be disruptive to the industry, Crist said. He estimates companies will spend upward of $500 million to comply with the new EPA rules and could struggle to meet the agency’s 18-month timetable. Sterilization companies will also have difficulty adjusting to new rules on how workers handle the gas without a dip in efficiency, Crist said.
The Food and Drug Administration, which regulates drugs and medical devices, is also watching the regulatory moves closely and worries the updated emissions rule could “present some unique challenges” if implemented as proposed, said Audra Harrison, an FDA spokesperson. “The FDA is concerned about the rule’s effects on the availability of medical devices,” she added.
Other groups, like the American Chemistry Council and the Texas Commission on Environmental Quality, the state’s environmental agency, assert that ethylene oxide use isn’t as dangerous as the EPA says. The EPA’s toxicity assessment has “severe flaws” and is “overly conservative,” the council said in an emailed statement. Texas, which has several sterilizing plants, has said ethylene oxide isn’t as high a cancer risk as the agency claims, an assessment that the EPA has rejected.
Tracey Woodruff, a researcher at the University of California-San Francisco who previously worked at the EPA, said it can be hard for the agency to keep up with regulating chemicals like ethylene oxide because of constrained resources, the technical complications of rulemaking, and industry lobbying.
But she’s hopeful the EPA can strike a balance between its desire to reduce exposure and the desire of the FDA not to disrupt medical device sterilization. And scrutiny can also help the device sterilization industry think outside the box.
“We continue to discover these chemicals that we’ve already been exposed to were toxic, and we have high exposures,” she said. “Regulation is an innovation forcer.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
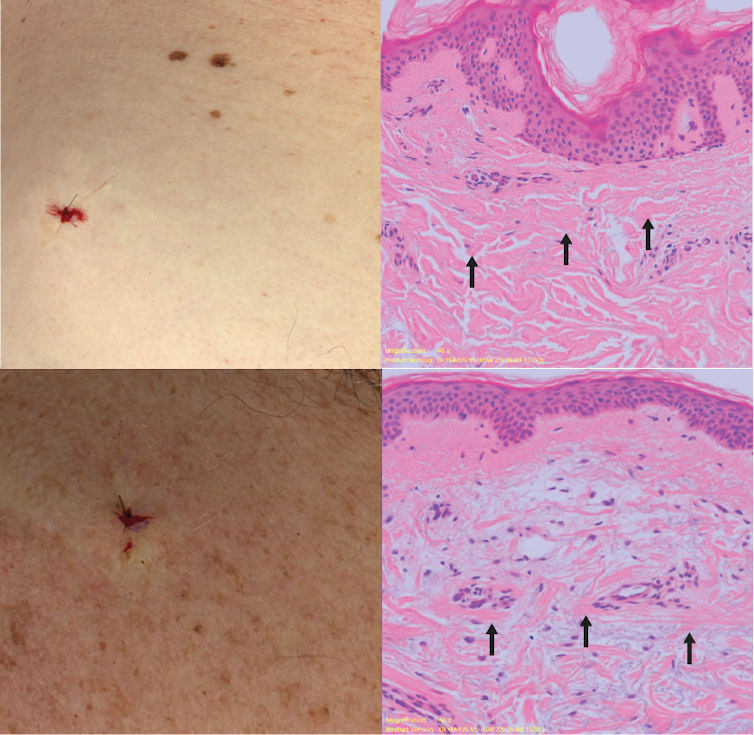
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
America Worries About Health Costs — And Voters Want to Hear From Biden and Republicans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
President Joe Biden is counting on outrage over abortion restrictions to help drive turnout for his reelection. Former President Donald Trump is promising to take another swing at repealing Obamacare.
But around America’s kitchen tables, those are hardly the only health topics voters want to hear about in the 2024 campaigns. A new KFF tracking poll shows that health care tops the list of basic expenses Americans worry about — more than gas, food, and rent. Nearly 3 in 4 adults — and majorities of both parties — say they’re concerned about paying for unexpected medical bills and other health costs.
“Absolutely health care is something on my mind,” Rob Werner, 64, of Concord, New Hampshire, said in an interview at a local coffee shop in January. He’s a Biden supporter and said he wants to make sure the Affordable Care Act, also known as Obamacare, is retained and that there’s more of an effort to control health care costs.
The presidential election is likely to turn on the simple question of whether Americans want Trump back in the White House. (Nikki Haley, the former South Carolina governor and U.S. ambassador to the United Nations, remained in the race for the Republican nomination ahead of Super Tuesday, though she had lost the first four primary contests.) And neither major party is basing their campaigns on health care promises.
But in the KFF poll, 80% of adults said they think it’s “very important” to hear presidential candidates talk about what they’d do to address health care costs — a subject congressional and state-level candidates can also expect to address.
“People are most concerned about out-of-pocket expenses for health care, and rightly so,” said Andrea Ducas, vice president of health policy at the Center for American Progress, a Washington, D.C.-based progressive think tank.
Here’s a look at the major health care issues that could help determine who wins in November.
Abortion
Less than two years after the Supreme Court overturned the constitutional right to an abortion, it is shaping up to be the biggest health issue in this election.
That was also the case in the 2022 midterm elections, when many voters rallied behind candidates who supported abortion rights and bolstered Democrats to an unexpectedly strong showing. Since the Supreme Court’s decision, voters in six states — including Kansas, Kentucky, and Ohio, where Republicans control the legislatures — have approved state constitutional amendments protecting abortion access.
Polls show that abortion is a key issue to some voters, said Robert Blendon, a public opinion researcher and professor emeritus at the Harvard T.H. Chan School of Public Health. He said up to 30% across the board see it as a “personal” issue, rather than policy — and most of those support abortion rights.
“That’s a lot of voters, if they show up and vote,” Blendon said.
Proposals to further protect — or restrict — abortion access could drive voter turnout. Advocates are working to put abortion-related measures on the ballot in such states as Arizona, Florida, Missouri, and South Dakota this November. A push in Washington toward a nationwide abortion policy could also draw more voters to the polls, Blendon said.
A surprise ruling by the Alabama Supreme Court in February that frozen embryos are children could also shake up the election. It’s an issue that divides even the anti-abortion community, with some who believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and others believing that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have children.
Pricey Prescriptions
Drug costs regularly rank high among voters’ concerns.
In the latest tracking poll, more than half — 55% — said they were very worried about being able to afford prescription drugs.
Biden has tried to address the price of drugs, though his efforts haven’t registered with many voters. While its name doesn’t suggest landmark health policy, the Inflation Reduction Act, or IRA, which the president signed in August 2022, included a provision allowing Medicare to negotiate prices for some of the most expensive drugs. It also capped total out-of-pocket spending for prescription drugs for all Medicare patients, while capping the price of insulin for those with diabetes at $35 a month — a limit some drugmakers have extended to patients with other kinds of insurance.
Drugmakers are fighting the Medicare price negotiation provision in court. Republicans have promised to repeal the IRA, arguing that forcing drugmakers to negotiate lower prices on drugs for Medicare beneficiaries would amount to price controls and stifle innovation. The party has offered no specific alternative, with the GOP-led House focused primarily on targeting pharmacy benefit managers, the arbitrators who control most Americans’ insurance coverage for medicines.
Costs of Coverage
Health care costs continue to rise for many Americans. The cost of employer-sponsored health plans have hit new highs in the past few months, raising costs for employers and workers alike. Experts have attributed the increase to high demand and expensive prices for certain drugs and treatments, notably weight loss drugs, as well as to medical inflation.
Meanwhile, the ACA is popular. The KFF poll found that more adults want to see the program expanded than scaled back. And a record 21.3 million people signed up for coverage in 2024, about 5 million of them new customers.
Enrollment in Republican-dominated states has grown fastest, with year-over-year increases of 80% in West Virginia, nearly 76% in Louisiana, and 62% in Ohio, according to the Centers for Medicare & Medicaid Services.
Public support for Obamacare and record enrollment in its coverage have made it politically perilous for Republicans to pursue the law’s repeal, especially without a robust alternative. That hasn’t stopped Trump from raising that prospect on the campaign trail, though it’s hard to find any other Republican candidate willing to step out on the same limb.
“The more he talks about it, the more other candidates have to start answering for it,” said Jarrett Lewis, a partner at Public Opinion Strategies, a GOP polling firm.
“Will a conversation about repeal-and-replace resonate with suburban women in Maricopa County?” he said, referring to the populous county in Arizona known for being a political bellwether. “I would steer clear of that if I was a candidate.”
Biden and his campaign have pounced on Trump’s talk of repeal. The president has said he wants to make permanent the enhanced premium subsidies he signed into law during the pandemic that are credited with helping to increase enrollment.
Republican advisers generally recommend that their candidates promote “a market-based system that has the consumer much more engaged,” said Lewis, citing short-term insurance plans as an example. “In the minds of Republicans, there is a pool of people that this would benefit. It may not be beneficial for everyone, but attractive to some.”
Biden and his allies have criticized short-term insurance plans — which Trump made more widely available — as “junk insurance” that doesn’t cover care for serious conditions or illnesses.
Entitlements Are Off-Limits
Both Medicaid and Medicare, the government health insurance programs that cover tens of millions of low-income, disabled, and older people, remain broadly popular with voters, said the Democratic pollster Celinda Lake. That makes it unlikely either party would pursue a platform that includes outright cuts to entitlements. But accusing an opponent of wanting to slash Medicare is a common, and often effective, campaign move.
Although Trump has said he wouldn’t cut Medicare spending, Democrats will likely seek to associate him with other Republicans who support constraining the program’s costs. Polls show that most voters oppose reducing any Medicare benefits, including by raising Medicare’s eligibility age from 65. However, raising taxes on people making more than $400,000 a year to shore up Medicare’s finances is one idea that won strong backing in a recent poll by The Associated Press and NORC Center for Public Affairs Research.
Brian Blase, a former Trump health adviser and the president of Paragon Health Institute, said Republicans, if they win more control of the federal government, should seek to lower spending on Medicare Advantage — through which commercial insurers provide benefits — to build on the program’s efficiencies and ensure it costs taxpayers less than the traditional program.
So far, though, Republicans, including Trump, have expressed little interest in such a plan. Some of them are clear-eyed about the perils of running on changing Medicare, which cost $829 billion in 2021 and is projected to consume nearly 18% of the federal budget by 2032.
“It’s difficult to have a frank conversation with voters about the future of the Medicare program,” said Lewis, the GOP pollster. “More often than not, it backfires. That conversation will have to happen right after a major election.”
Addiction Crisis
Many Americans have been touched by the growing opioid epidemic, which killed more than 112,000 people in the United States in 2023 — more than gun deaths and road fatalities combined. Rural residents and white adults are among the hardest hit.
Federal health officials have cited drug overdose deaths as a primary cause of the recent drop in U.S. life expectancy.
Republicans cast addiction as largely a criminal matter, associating it closely with the migration crisis at the U.S. southern border that they blame on Biden. Democrats have sought more funding for treatment and prevention of substance use disorders.
“This affects the family, the neighborhood,” said Blendon, the public opinion researcher.
Billions of dollars have begun to flow to states and local governments from legal settlements with opioid manufacturers and retailers, raising questions about how to best spend that money. But it isn’t clear that the crisis, outside the context of immigration, will emerge as a campaign issue.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Major Chronic Diseases – by Alexis Dupree
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our author, Alexis Dupree, is herself in her 70s, and writing with more than three decades of experience of surviving multiple chronic diseases (in her case, Multiple Sclerosis, and then a dozen comorbidities that came with such).
She is not a doctor or a scientist, but for more than 30 years she’s been actively working to accumulate knowledge not just on her own conditions, but on the whole medical system, and what it means to be a “forever patient” without giving up hope.
She talks lived-experience “life management” strategies for living with chronic disease, and she talks—again from lived experience—about navigating the complexities of medical care; not on a legalistic “State regulations say…” level, because that kind of thing changes by the minute, but on a human level.
Perhaps most practically: how to advocate strongly for yourself while still treating medical professionals with the respect and frankly compassion that they deserve while doing their best in turn.
But also: how to change your attitude to that of a survivor, and yet also redefine your dreams. How to make a new game plan of life—while working to make life easier for yourself. How to deal, psychologically, with the likelihood that not only will you probably not get better, but also, you will probably get worse, while still never, ever, giving up.
After all, many things are easily treatable today that mere decades ago were death sentences, and science is progressing all the time. We just have to stay alive, and in as good a condition as we reasonably can, to benefit from those advances!
Bottom line: if you have a chronic disease, or if a loved one does, then this is an immensely valuable book to read.
Click here to check out Managing Major Chronic Diseases, and make life easier!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: