Debate over tongue tie procedures in babies continues. Here’s why it can be beneficial for some infants
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is increasing media interest about surgical procedures on new babies for tongue tie. Some hail it as a miracle cure, others view it as barbaric treatment, though adverse outcomes are rare.
Tongue tie occurs when the tissue under the tongue is attached to the lower gum or floor of the mouth in a way that can restrict the movement or range of the tongue. This can impact early breastfeeding in babies. It affects an estimated 8% of children under one year of age.
While there has been an increase in tongue tie releases (also called division or frenotomy), it’s important to keep this in perspective relative to the increase in breastfeeding rates.
The World Health Organization recommends exclusive breastfeeding for the first six months of life, with breastfeeding recommended into the second year of life and beyond for the health of mother and baby as well as optimal growth. Global rates of breastfeeding infants for the first six months have increased from 38% to 48% over the past decade. So, it is not surprising there is also an increase in the number of babies being referred globally with breastfeeding challenges and potential tongue tie.
An Australian study published in 2023 showed that despite a 25% increase in referrals for tongue tie division between 2014 and 2018, there was no increase in the number of tongue tie divisions performed. Tongue tie surgery rates increased in Australia in the decade from 2006 to 2016 (from 1.22 per 1,000 population to 6.35) for 0 to 4 year olds. There is no data on surgery rates in Australia over the last eight years.
Tongue tie division isn’t always appropriate but it can make a big difference to the babies who need it. More referrals doesn’t necessarily mean more procedures are performed.

How tongue tie can affect babies
When tongue tie (ankyloglossia) restricts the movement of the tongue, it can make it more difficult for a baby to latch onto the mother’s breast and painlessly breastfeed.
Earlier this month, the International Consortium of oral Ankylofrenula Professionals released a tongue tie position statement and practice guideline. Written by a range of health professionals, the guidelines define tongue tie as a functional diagnosis that can impact breastfeeding, eating, drinking and speech. The guidelines provide health professionals and families with information on the assessment and management of tongue tie.
Tongue tie release has been shown to improve latch during breastfeeding, reduce nipple pain and improve breast and bottle feeding. Early assessment and treatment are important to help mothers breastfeed for longer and address any potential functional problems.

Where to get advice
If feeding isn’t going well, it may cause pain for the mother or there may be signs the baby isn’t attaching properly to the breast or not getting enough milk. Parents can seek skilled help and assessment from a certified lactation consultant or International Board-Certified Lactation Consultant who can be found via online registry.
Alternatively, a health professional with training and skills in tongue tie assessment and division can assist families. This may include a doctor, midwife, speech pathologist or dentist with extended skills, training and experience in treating babies with tongue tie.
When access to advice or treatment is delayed, it can lead to unnecessary supplementation with bottle feeds, early weaning from breastfeeding and increased parental anxiety.
Getting a tongue tie assessment
During assessment, a qualified health professional will collect a thorough case history, including pregnancy and birth details, do a structural and functional assessment, and conduct a comprehensive breastfeeding or feeding assessment.
They will view and thoroughly examine the mouth, including the tongue’s movement and lift. The appearance of where the tissue attaches to the underside of the tongue, the ability of the tongue to move and how the baby can suck also needs to be properly assessed.
Treatment decisions should focus on the concerns of the mother and baby and the impact of current feeding issues. Tongue tie division as a baby is not recommended for the sole purpose of avoiding speech problems in later life if there are no feeding concerns for the baby.

Treatment options
The Australian Dental Association’s 2020 guidelines provide a management pathway for babies diagnosed with tongue tie.
Once feeding issues are identified and if a tongue tie is diagnosed, non-surgical management to optimise positioning, latch and education for parents should be the first-line approach.
If feeding issues persist during follow-up assessment after non-surgical management, a tongue tie division may be considered. Tongue tie release may be one option to address functional challenges associated with breastfeeding problems in babies.
There are risks associated with any procedure, including tongue tie release, such as bleeding. These risks should be discussed with the treating practitioner before conducting any laser, scissor or scalpel tongue tie procedure.
Post-release support by a certified lactation consultant or feeding specialist is necessary after a tongue tie division. A post-release treatment plan should be developed by a team of health professionals including advice and support for breastfeeding to address both the mother and baby’s individual needs.
We would like to acknowledge the contribution of Raymond J. Tseng, DDS, PhD, (Paediatric Dentist) to the writing of this article.
Sharon Smart, Lecturer and Researcher (Speech Pathology) – School of Allied Health, Curtin University; David Todd, Associate Professor, Neonatology, ANU Medical School, Australian National University, and Monica J. Hogan, PhD student, ANU School of Medicine and Psychology, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
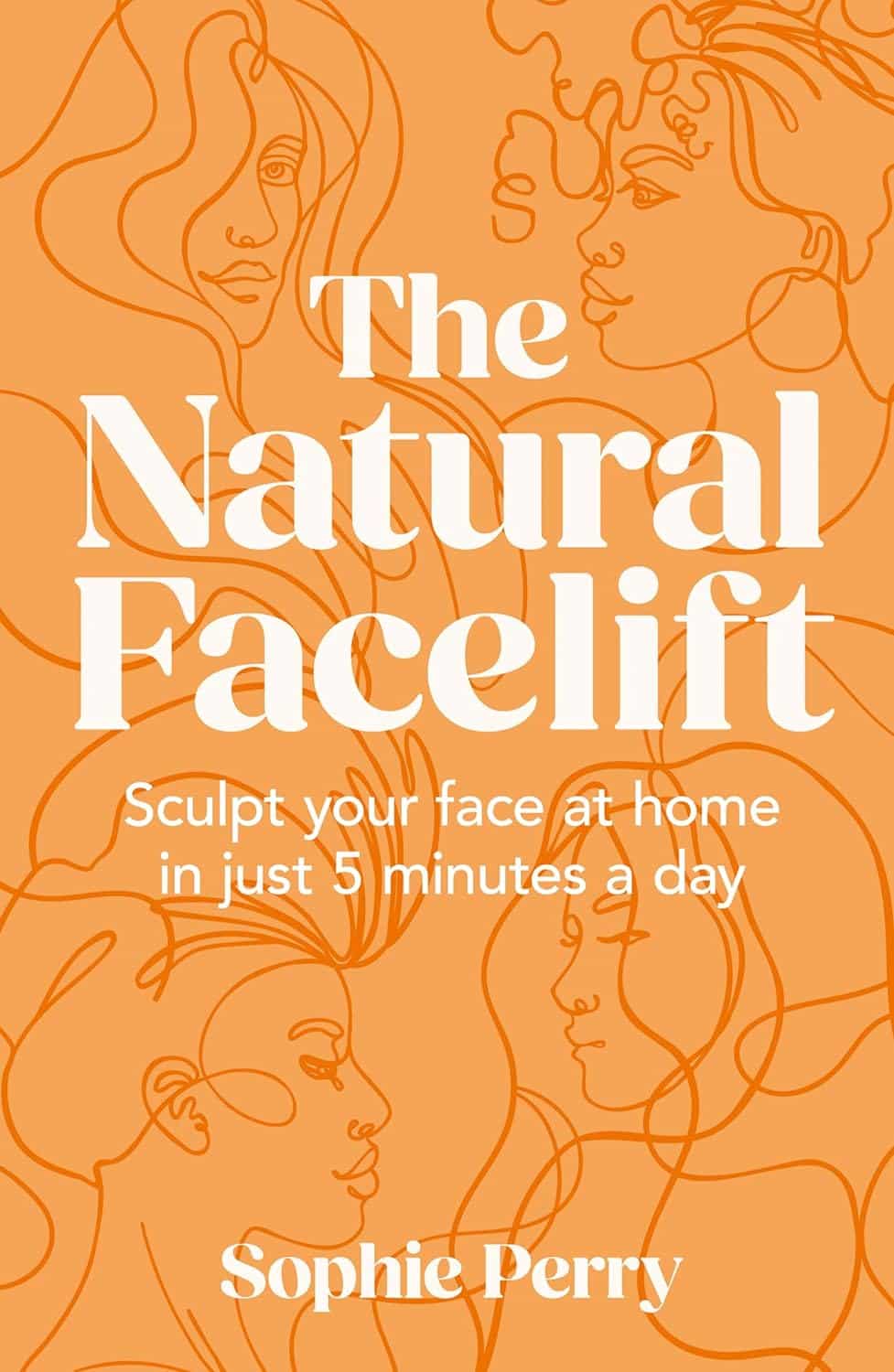
The Natural Facelift – by Sophie Perry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book isn’t: it’s mostly not about beauty, and it’s certainly not about ageist ideals of “hiding” aging.
The author herself discusses the privilege that is aging (not everyone gets to do it) and the importance of taking thankful pride in our lived-in bodies.
The title and blurb belie the contents of the book rather. Doubtlessly the publisher felt that extrinsic beauty would sell better than intrinsic wellbeing. As for what it’s actually more about…
Ever splashed your face in cold water to feel better? This book’s about revitalising the complex array of facial muscles (there are anatomical diagrams) and the often-tired and very diverse tissues that cover them, complete with the array of nerve endings very close to your CNS (not to mention the vagus nerve running just behind your jaw), and some of the most important blood vessels of your body, serving your brain.
With all that in mind, this book, full of useful therapeutic techniques, is a very, very far cry from “massage like this and you’ll look like you got photoshopped”.
The style varies, as some parts of explanation of principles, or anatomy, and others are hands-on (literally) guides to the exercises, but it is all very clear and easy to understand/follow.
Bottom line: aspects of conventional beauty may be a side-effect of applying the invigorating exercises described in this book. The real beauty is—literally—more than skin-deep.
Click here to check out The Natural Facelift, and order yours!
Share This Post
-
15 Easy Japanese Habits That Will Transform Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The original title says “no-cost habits”, but in fairness, for most of us food is not usually free (alas). So, we will say “easy” instead, because they are indeed easy to build into your life:
15 Healthy Habits To Adopt
We’ll not keep them a mystery; they are:
- Intermittent fasting: naturally fasting for at least 12 hours overnight improves digestion and sleep quality.
- Fermented foods: regularly consuming fermented foods (like kimchi, or even just sauces like miso and shio koji) supports gut health.
- Rice & legumes over wheat: choosing wholegrain rice as a staple reduces bloating and benefits skin health (lentils are even better).
- Big breakfast, light dinner: eating a heavier breakfast and a lighter dinner gives energy in the morning and allows digestion to rest at night.
- Balancing indulgences: enjoying social meals without guilt and balancing food intake the next day.
- Daily gentle exercise: doing at least 15 minutes of yoga, Pilates, or light walking for long-term health.
- Daily baths: taking a warm bath boosts blood circulation and relaxation.
- Eating seasonal & diverse foods: including a variety of fresh, seasonal ingredients for balanced nutrition.
- Consistent morning routine: waking up at the same time, cleansing and moisturizing, and having a proper breakfast.
- Enjoying soup with meals: consuming nutrient-rich soups with vegetables and protein to prevent overeating.
- Chewing food thoroughly: eating slowly and chewing well aids digestion and enhances enjoyment.
- Light seasoning in food: avoiding overly salty or flavorful meals to appreciate natural tastes.
- Maintaining good posture: paying attention to posture during daily activities for better overall health.
- Prioritizing protein intake: eating protein-rich foods like tofu, beans, eggs, and fish, to maintain skin firmness as well as muscletone.
- Confidence in aging: focusing on internal well-being over external opinions and embracing health at every age.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Share This Post
-
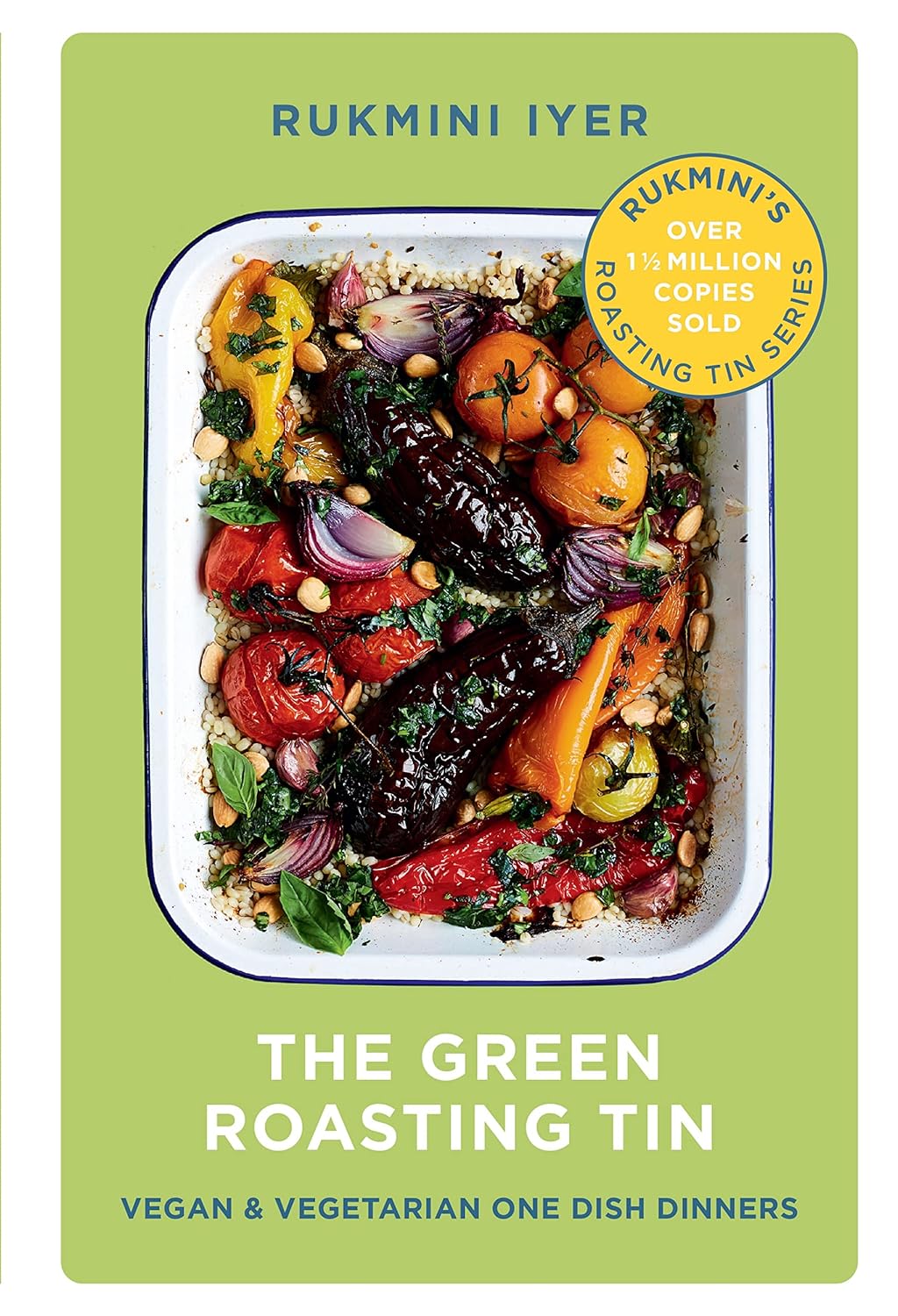
The Green Roasting Tin – by Rukmini Iyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: “do I really need a book to tell me to put some vegetables in a roasting tin and roast them?” and maybe not, but the book offers a lot more than that.
Indeed, the author notes “this book was slightly in danger of becoming the gratin and tart book, because I love both”, but don’t worry, most of the recipes are—as you might expect—very healthy.
As for formatting: the 75 recipes are divided first into vegan or vegetarian, and then into quick/medium/slow, in terms of how long they take.
However, even the “slow” recipes don’t actually take more effort, just, more time in the oven.
One of the greatest strengths of this book is that not only does it offer a wide selection of wholesome mains, but also, if you’re putting on a big spread, these can easily double up as high-class low-effort sides.
Bottom line: if you’d like to eat more vegetables in 2024 but want to make it delicious and with little effort, put this book on your Christmas list!
Click here to check out The Green Roasting Tin, and level-up yours!
Share This Post
Related Posts
-
Thinking of using an activity tracker to achieve your exercise goals? Here’s where it can help – and where it probably won’t
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of year when many people are getting started on their resolutions for the year ahead. Doing more physical activity is a popular and worthwhile goal.
If you’re hoping to be more active in 2024, perhaps you’ve invested in an activity tracker, or you’re considering buying one.
But what are the benefits of activity trackers? And will a basic tracker do the trick, or do you need a fancy one with lots of features? Let’s take a look.
Why use an activity tracker?
One of the most powerful predictors for being active is whether or not you are monitoring how active you are.
Most people have a vague idea of how active they are, but this is inaccurate a lot of the time. Once people consciously start to keep track of how much activity they do, they often realise it’s less than what they thought, and this motivates them to be more active.
You can self-monitor without an activity tracker (just by writing down what you do), but this method is hard to keep up in the long run and it’s also a lot less accurate compared to devices that track your every move 24/7.
By tracking steps or “activity minutes” you can ascertain whether or not you are meeting the physical activity guidelines (150 minutes of moderate to vigorous physical activity per week).
It also allows you to track how you’re progressing with any personal activity goals, and view your progress over time. All this would be difficult without an activity tracker.
Research has shown the most popular brands of activity trackers are generally reliable when it comes to tracking basic measures such as steps and activity minutes.
But wait, there’s more
Many activity trackers on the market nowadays track a range of other measures which their manufacturers promote as important in monitoring health and fitness. But is this really the case? Let’s look at some of these.
Resting heart rate
This is your heart rate at rest, which is normally somewhere between 60 and 100 beats per minute. Your resting heart rate will gradually go down as you become fitter, especially if you’re doing a lot of high-intensity exercise. Your risk of dying of any cause (all-cause mortality) is much lower when you have a low resting heart rate.
So, it is useful to keep an eye on your resting heart rate. Activity trackers are pretty good at tracking it, but you can also easily measure your heart rate by monitoring your pulse and using a stopwatch.
Heart rate during exercise
Activity trackers will also measure your heart rate when you’re active. To improve fitness efficiently, professional athletes focus on having their heart rate in certain “zones” when they’re exercising – so knowing their heart rate during exercise is important.
But if you just want to be more active and healthier, without a specific training goal in mind, you can exercise at a level that feels good to you and not worry about your heart rate during activity. The most important thing is that you’re being active.
Also, a dedicated heart rate monitor with a strap around your chest will do a much better job at measuring your actual heart rate compared to an activity tracker worn around your wrist.
Maximal heart rate
This is the hardest your heart could beat when you’re active, not something you could sustain very long. Your maximal heart rate is not influenced by how much exercise you do, or your fitness level.
Most activity trackers don’t measure it accurately anyway, so you might as well forget about this one.
VO₂max
Your muscles need oxygen to work. The more oxygen your body can process, the harder you can work, and therefore the fitter you are.
VO₂max is the volume (V) of oxygen (O₂) we could breathe maximally (max) over a one minute interval, expressed as millilitres of oxygen per kilogram of body weight per minute (ml/kg/min). Inactive women and men would have a VO₂max lower than 30 and 40 ml/kg/min, respectively. A reasonably good VO₂max would be mid thirties and higher for women and mid forties and higher for men.
VO₂max is another measure of fitness that correlates well with all-cause mortality: the higher it is, the lower your risk of dying.
For athletes, VO₂max is usually measured in a lab on a treadmill while wearing a mask that measures oxygen consumption. Activity trackers instead look at your running speed (using a GPS chip) and your heart rate and compare these measures to values from other people.
If you can run fast with a low heart rate your tracker will assume you are relatively fit, resulting in a higher VO₂max. These estimates are not very accurate as they are based on lots of assumptions. However, the error of the measurement is reasonably consistent. This means if your VO₂max is gradually increasing, you are likely to be getting fitter.
So what’s the take-home message? Focus on how many steps you take every day or the number of activity minutes you achieve. Even a basic activity tracker will measure these factors relatively accurately. There is no real need to track other measures and pay more for an activity tracker that records them, unless you are getting really serious about exercise.
Corneel Vandelanotte, Professorial Research Fellow: Physical Activity and Health, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The #1 Foot Health Secret Everyone Over 50 Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite over-50s specialist physio Will Harlow is here to keep us on our toes:
Mobility requires mobilization
As we age, our toes are inclined to become stiffer. Stiff toes lead to balance issues and increased risk of falling.
A study cited in the video showed that two weeks of toe mobilization improved foot-ground contact by 30% in older adults, enhancing balance and reducing falls.
Here’s the routine:
- Toe flexion:
- Apply moisturizer or oil to your hands.
- Pull your toes downwards, then let them return their normal position.
- Repeat for one minute per foot.
- Toe extension:
- Rub hands from the heel under the toes.
- Push your toes upwards, then let them return to their normal position.
- Repeat for one minute per foot.
- Foot rotation:
- Hold both sides of your foot and twist it in one direction, then the other.
- This helps loosen foot joints and improve flexibility.
- Perform for one minute in each direction per foot.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Toe flexion:
-
Top Foods Against Neuroinflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is something you might feel in your joints, but it will usually be in the brain too. There, neuroinflammation can disrupt brain function, affecting stress responses, mood, cognition, and even alter brain structure. It’s also heavily implicated in the pathogenesis of various forms of dementia.
What to do about it
Dr. Tracey Marks, psychiatrist, bids us eat:
- Fatty fish: omega-3-rich fish like salmon reduce neuroinflammation.
- Leafy greens: spinach, kale, and collards protect brain cells and support neurotransmitter production.
- Berries: blueberries and strawberries improve memory and protect neurons.
- Nuts and seeds: walnuts, almonds, and flaxseeds support brain health and reduce inflammation.
- Turmeric: curcumin combats inflammation and supports neuron growth (best with supplements).
- Fermented foods: yogurt and sauerkraut improve gut health, benefiting the brain via the gut-brain axis; not just the vagus nerve, but also, remember that various neurotransmitters (including serotonin) are made in the gut.
Of course, you should also avoid alcohol, nicotine, red meat, processed meat, and ideally also white flour products, and sugary foods (unless they are also rich in fiber, like whole fruit).
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: