The BAT-pause!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Cold Weather & The Menopause Battle It Out
You may know that (moderate, safe) exposure to the cold allows our body to convert our white and yellow fat into the much healthier brown fat—also called brown adipose tissue, or “BAT” to its friends.
If you didn’t already know that, then well, neither did scientists until about 15 years ago:
The Changed Metabolic World with Human Brown Adipose Tissue: Therapeutic Visions
You can read more about it here:
Cool Temperature Alters Human Fat and Metabolism
This is important, especially because the white fat that gets converted is the kind that makes up most visceral fat—the kind most associated with all-cause mortality:
Visceral Belly Fat & How To Lose It ← this is not the same as your subcutaneous fat, the kind that sits directly under your skin and keeps you warm; this is the fat that goes between your organs and of which we should only have a small amount!
The BAT-pause
It’s been known (since before the above discovery) that BAT production slows considerably as we get older. Not too shocking—after all, many metabolic functions slow as we get older, so why should fat regulation be any different?
But! Rodent studies found that this was tied less to age, but to ovarian function: rats who underwent ovariectomies suffered reduced BAT production, regardless of their age.
Naturally, it’s been difficult to recreate such studies in humans, because it’s difficult to find a large sample of young adults willing to have their ovaries whipped out (or even suppressed chemically) to see how badly their metabolism suffers as a result.
Nor can an observational study (for example, of people who incidentally have ovaries removed due to ovarian cancer) usefully be undertaken, because then the cancer itself and any additional cancer treatments would be confounding factors.
Perimenopausal study to the rescue!
A recent (published last month, at time of writing!) study looked at women around the age of menopause, but specifically in cohorts before and after, measuring BAT metabolism.
By dividing the participants into groups based on age and menopausal status, and dividing the post-menopausal group into “takes HRT” and “no HRT” groups, and dividing the pre-menopausal group into “normal ovarian function” and “ovarian production of estrogen suppressed to mimic slightly early menopause” groups (there’s a drug for that), and then having groups exposed to warm and cold temperatures, and measuring BAT metabolism in all cases, they were able to find…
It is about estrogen, not age!
You can read more about the study here:
“Good” fat metabolism changes tied to estrogen loss, not necessarily to aging, shows study
…and the study itself, here:
Brown adipose tissue metabolism in women is dependent on ovarian status
What does this mean for men?
This means nothing directly for (cis) men, sorry.
But to satisfy your likely curiosity: yes, testosterone does at least moderately suppress BAT metabolism—based on rodent studies, anyway, because again it’s difficult to find enough human volunteers willing to have their testicles removed for science (without there being other confounding variables in play, anyway):
Testosterone reduces metabolic brown fat activity in male mice
So, that’s bad per se, but there isn’t much to be done about it, since the rest of your (addressing our male readers here) metabolism runs on testosterone, as do many of your bodily functions, and you would suffer many unwanted effects without it.
However, as men do typically have notably less body fat in general than women (this is regulated by hormones), the effects of changes in BAT metabolism are rather less pronounced in men (per testosterone level changes) than in women (per estrogen level changes), because there’s less overall fat to convert.
In summary…
While menopausal HRT is not necessarily a silver bullet to all metabolic problems, its BAT-maintaining ability is certainly one more thing in its favor.
See also:
Dr. Jen Gunter | What You Should Have Been Told About The Menopause Beforehand
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ageless Athletes – by Dr. Jim Madden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an approach to strength and fitness training specifically for the 50+ crowd, and/but even more specifically for the 50+ crowd who do not wish to settle for mediocrity. In short, it’s for those who not only wish to stay healthy and have good mobility, but also who wish to be and remain athletic.
It does not assume extant athleticism, but nor does it assume complete inexperience. It provides a fairly ground-upwards entry to a training program that then quickly proceeds to competitive levels of athleticism.
The author himself details his own journey from being in his 30s, overweight and unfit, to being in his 50s and very athletic, with before and after photos. Granted, those are 20 years in between, but all the same, it’s a good sign when someone gets stronger and fitter with age, rather than declining.
The style of the book is quite casual, and/but after the introductory background and pep talk, is quite pragmatic and drops the additional fluff. In particular, older readers may enjoy the “Old Workhorse” protocol, as a tailored measured progression system.
In terms of expected equipment by the way, some is bodyweight and some is with weights; kettlebells in particular feature strongly, since this is about functional strength and not bodybuilding.
In the category of criticism, he does refer to his other books and generally assumes the reader is reading all his work, so it may not be for everyone as a standalone book.
Bottom line: if you’re 50+ and are wondering how to gain/maintain a high level athleticism, this book can definitely help with that.
Click here to check out Ageless Athlete, and go from strength to strength!
Share This Post
-
Body by Science – by Dr. Doug McGuff & John Little
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The idea that you’ll get a re-sculpted body at 12 minutes per week is a bold claim, isn’t it? Medical Doctor Doug McGuff and bodybuilder John Little team up to lay out their case. So, how does it stand up to scrutiny?
First, is it “backed by rigorous research” as claimed? Yes… with caveats.
The book uses a large body of scientific literature as its foundation, and that weight of evidence does support this general approach:
- Endurance cardio isn’t very good at burning fat
- Muscle, even just having it without using it much, burns fat to maintain it
- To that end, muscle can be viewed as a fat-burning asset
- Muscle can be grown quickly with short bursts of intense exercise once per week
Why once per week? The most relevant muscle fibers take about that long to recover, so doing it more often will undercut gains.
So, what are the caveats?
The authors argue for slow reps of maximally heavy resistance work sufficient to cause failure in about 90 seconds. However, most of the studies cited for the benefits of “brief intense exercise” are for High Intensity Interval Training (HIIT). HIIT involves “sprints” of exercise. It doesn’t have to be literally running, but for example maxing out on an exercise bike for 30 seconds, slowing for 60, maxing out for 30, etc. Or in the case of resistance work, explosive (fast!) concentric movements and slow eccentric movements, to work fast- and slow-twitch muscle fibers, respectively.
What does this mean for the usefulness of the book?
- Will it sculpt your body as described in the blurb? Yes, this will indeed grow your muscles with a minimal expenditure of time
- Will it improve your body’s fat-burning metabolism? Yes, this will indeed turn your body into a fat-burning machine
- Will it improve your “complete fitness”? No, if you want to be an all-rounder athlete, you will still need HIIT, as otherwise anything taxing your under-worked fast-twitch muscle fibers will exhaust you quickly.
Bottom line: read this book if you want to build muscle efficiently, and make your body more efficient at burning fat. Best supplemented with at least some cardio, though!
Click here to check out Body by Science, and get re-sculpting yours!
Share This Post
-
This Is Your Brain on Music – by Dr. Daniel Levitin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Music has sometimes been touted as having cognitive benefits, by its practice and even by the passive experience of it. But what’s the actual science of it?
Dr. Levitin, an accomplished musician and neuroscientist, explores and explains.
We learn about how music in all likelihood allowed our ancestors to develop speech, something that set us apart (and ahead!) as a species. How music was naturally-selected-for in accordance with its relationship with health. How processing music involves almost every part of the brain. How music pertains specifically to memory. And more.
As a bonus, as well as explaining a lot about our brain, this book offers those of us with limited knowledge of music theory a valuable overview of the seven main dimensions of music, too.
Bottom line: if you’d like to know more about the many-faceted relationship between music and cognitive function, this is a top-tier book about such.
Click here to check out “This Is Your Brain On Music”, and learn more about yours!
Share This Post
Related Posts
-
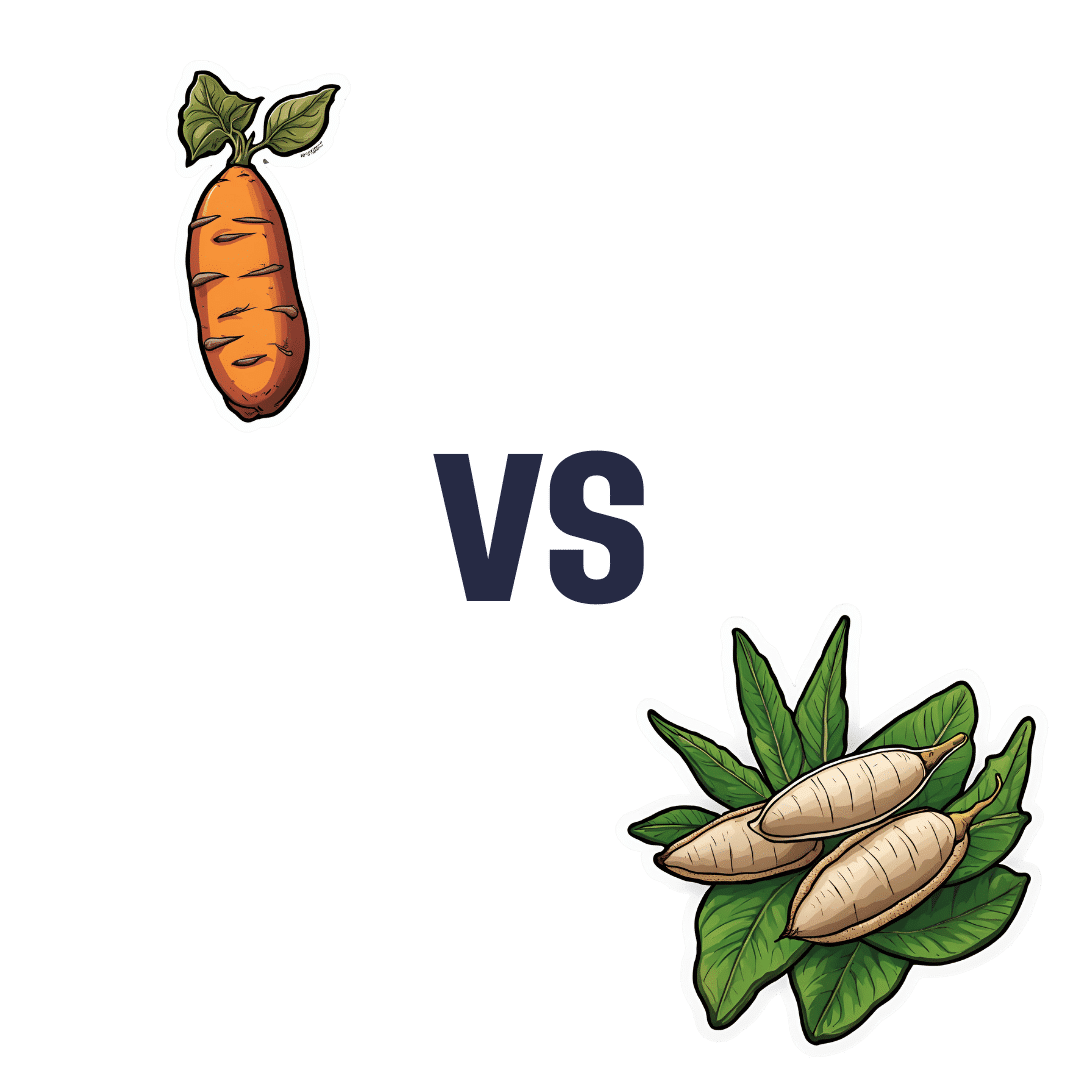
Sweet Potato vs Cassava – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sweet potato to cassava, we picked the sweet potato.
Why?
For any unfamiliar with cassava, it’s also called manioc or yuca/yucca, and it’s a tuber that can be used a lot like sweet potato. It’s popular in S. America, often in recipes that aren’t the healthiest (deep-fried chunky “cassava chips” are popular in Brazil, for example, and farofa, a flour made from cassava, is less healthy even than refined white flour from wheat), but today we’re going to judge it on its own merit—since after all, almost anything can be deep-fried and many things can be turned into flour, but it doesn’t mean we have to do that.
Let’s talk macros first: sweet potato has nearly 2x the protein, while cassava has nearly 2x the carbs. As for fiber to soften those carbs’ impact on our blood sugars, well, sweet potato has about 2x the fiber. All in all for macros, a clear and easy win for sweet potato.
Important note: as for the impact that has on glycemic index: the exact glycemic index will depend on what you do with it (different cooking methods change the GI), but broadly speaking, sweet potatoes are considered a medium GI food, while cassava is a very high GI food, to the point that it’s higher than sucrose, and nearly equal to pure glucose. Which is impressive, for a tuber.
In terms of vitamins, sweet potato’s famously high vitamin A content raises the bar, but it’s not all it has to offer: sweet potato has more of vitamins A, B1, B2, B3, B5, B6, E, and K, while cassava has more of vitamins B9 and choline. Just for amusement’s sake, let’s note that the sweet potato has over 1,478x the vitamin A content. In any case, the vitamins category is another clear win for sweet potato.
When it comes to minerals, it’s again quite one-sided: sweet potato has more calcium, copper, iron, magnesium, manganese, phosphorus, and potassium, while cassava has more selenium. So, sweet potato wins yet again.
In short: definitely a case of “the less widely-available option is not necessarily the healthier”!
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pine Nuts vs Macadamia Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to macadamias, we picked the pine nuts.
Why?
In terms of macros, it’s subjective depending on what you want to prioritize; the two nuts are equal in carbs, but pine nuts have more protein and macadamias have more fiber. We’d generally prioritize the fiber, which so far would give macadamias a win in this category, but if you prefer the protein, then consider it pine nuts. Next, we must consider fats; macadamias have slightly more fat, and of which, proportionally more saturated fat, resulting in 3x the total saturated fat compared to pine nuts, gram for gram. With this in mind, we consider this category a tie or a marginal nominal win for pine nuts.
In the category of vitamins, pine nuts have more of vitamins A, B2, B3, B9, E, K, and choline, while macadamias have more of vitamins B1, B5, B6, and C. A clear win for pine nuts this time, especially with pine nuts having more than 17x the vitamin E of macadamias.
When it comes to minerals, pine nuts have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while macadamias have more calcium and selenium. Another easy win for pine nuts.
In short, enjoy either or both (diversity is good), but pine nuts are the healthier by most metrics.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: