Fix Your Upper Back With These Three Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to back pain, the lower back gets a lot of attention, but what about when it’s nearer the neck and shoulders?
Reaching for better health
In this short video, Liv describes and shows three exercises:
Exercise 1: Thoracic Pullover (Dumbbell Pullover)
Purpose: Improves overhead reach and shoulder mobility.
Equipment: light weight, yoga block, or foam roller.
Steps:
- Lie on the floor with the foam roller/block beneath the upper back.
- Hold the weight in both hands, arms extended upward.
- Inhale deeply and reach the weight toward the ceiling.
- Exhale and arc your spine over the block, moving the weight backward.
- Keep core tension to maintain a neutral lower back position.
- Perform 10 repetitions.
Exercise 2: Rotational Mobility Stretch
Purpose: enhances torso rotation, core strength, and hip mobility.
Equipment: none (or a mat)
Steps:
- Lie on your side with knees stacked at 90° and arms extended in front.
- Hold a weight in the top hand.
- Inhale and lift the top arm toward the ceiling, extending the shoulder blade.
- Exhale and twist your torso, allowing the arm to move toward the floor.
- Modify by extending the bottom leg for a deeper twist if needed.
- Perform 6 reps per side, switching legs and repeating on the other side.
Exercise 3: Doorway/Pole Side Stretch
Purpose: targets multiple areas for a deep, satisfying stretch.
Equipment: door frame, pole, or wall.
Steps:
- Stand at arm’s length from the wall or frame.
- Cross the outer leg (furthest from the wall) behind the inner leg.
- Place the closest hand on the wall and reach the other arm overhead.
- Grip the wall or frame with the top hand, pressing away with the bottom hand.
- Lean into a banana-shaped curve and rotate your chest upward for a deeper stretch.
- Hold for 20–30 seconds per side and repeat 2–3 times.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 10 Foods That Promote Lymphatic Drainage and Lymph Flow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Melissa Gallagher, a naturopath by profession, recommends the following 10 foods that she says promote lymphatic drainage and lymph flow, as well as the below-mentioned additional properties:
Ginger
Ginger is a natural anti-inflammatory, which we wrote about here:
Ginger Does A Lot More Than You Think
Turmeric
Turmeric is another natural anti-inflammatory, which we wrote about here:
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Garlic
Garlic is—you guessed it—another natural anti-inflammatory which we wrote about here:
The Many Health Benefits Of Garlic
Pineapple
Pineapple contains a collection of enzymes collectively called bromelain—which is a unique kind of anti-inflammatory, and which we have written about here:
Bromelain vs Inflammation & Much More
Citrus
Citrus fruits like oranges, lemons, and grapefruits are rich in vitamin C, which can help support the immune system in general.
Cranberry
Cranberries contain antioxidants and anti-inflammatory compounds, which we wrote about here:
Health Benefits Of Cranberries (But: You’d Better Watch Out)
The video also explains how cranberry bioactives inhibit adipogenesis and reduces fat congestion in your lymphatic system.
Dandelion Tea
Dandelion is a natural diuretic and anti-inflammatory herb, which we’ve not written about yet!
Nettle Tea
Nettle is a natural diuretic and anti-inflammatory herb, which we’ve also not written about yet!
Healthy Fats
Healthy fats like avocado, nuts, and olive oil can help reduce inflammation and support the immune system.
Fermented Foods
Fermented foods, such as kimchi and sauerkraut, contain probiotics that can improve gut health, which in turn boosts the immune system. You can read all about it here:
Making Friends With Your Gut (You Can Thank Us Later)
Want the full explanation? Here’s the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Radiant Rebellion – by Karen Walrond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In health terms, we are often about fighting aging here. But to be more specific, what we’re fighting in those cases is not truly aging itself, so much as age-related decline.
Karen Walrond makes a case that we’ve made from the very start of 10almonds (but she wrote a whole book about it), that there’s merit in looking at what we can and can’t control about aging, doing what we reasonably can, and embracing what we can’t.
And yes, embracing, not merely accepting. This is not a downer of a book; it’s a call to revolution. It asks us to be proud of our grey hairs, to see our smile-lines around our eyes as the sign of a lived-in body, and even to embrace some of the unavoidable “actual decline” things as part of the journey of life. Maybe we’re not as strong as we used to be and now need a grippety-doodah to open jars; not everyone gets to live long enough to experience that! How lucky we are.
Perhaps most importantly, she bids us be the change we want to see in the world, and inspire others with our choices and actions, and shake off ageist biases for good.
Bottom line: if you want to foster a better attitude to aging not only for yourself, but also those around you, then this is a top-tier book for that.
Click here to check out Radiant Rebellion, and reclaim aging!
Share This Post
-
Ageless Aging – by Maddy Dychtwald
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maddy Dychtwald, herself 73, has spent her career working in the field of aging. She’s not a gerontologist or even a doctor, but she’s nevertheless been up-to-the-ears in the industry for decades, mostly as an organizer, strategist, facilitator, and so forth. As such, she’s had her finger on the pulse of the healthy longevity movement for a long time.
This book was written to address a problem, and the problem is: lifespan is increasing (especially for women), but healthspan has not been keeping up the pace.
In other words: people (especially women) are living longer, but often with more health problems along the way than before.
And mostly, it’s for lack of information (or sometimes: too much competing incorrect information).
Fortunately, information is something that a woman in Dychtwald’s position has an abundance of, because she has researchers and academics in many fields on speed-dial and happy to answer her questions (we get a lot of input from such experts throughout the book—which is why this book is so science-based, despite the author not being a scientist).
The book answers a lot of important questions beyond the obvious “what diet/exercise/sleep/supplements/etc are best for healthy aging” (spoiler: it’s quite consistent with the things we recommend here, because guess what, science is science), questions like how best to prepare for this that or the other, how to get a head start on preventative healthcare for some things, how to avoid being a burden to our families (one can argue that families are supposed to look after each other, but still, it’s a legitimate worry for many, and understandably so), and even how to balance the sometimes conflicting worlds of health and finances.
Unlike many authors, she also talks about the different kinds of aging, and tackles each of them separately and together. We love to see it!
Bottom line: this book is a very good one-stop-shop for all things healthy aging. It’s aimed squarely at women, but most advice goes for men the same too, aside from the section on hormones and such.
Click here to check out Ageless Aging, and plan your future!
Share This Post
Related Posts
-
Breast Milk’s Benefits That Are (So Far) Not Replicable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Simply The Breast 🎶
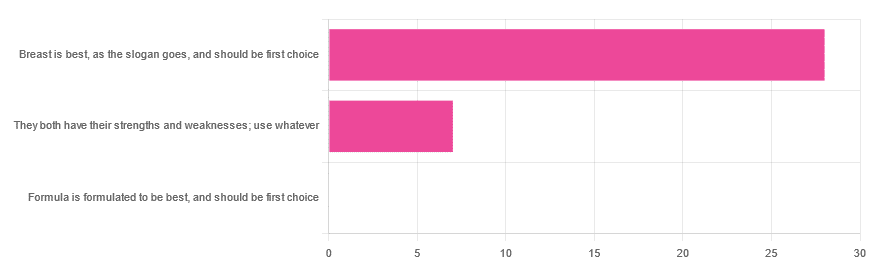
In Wednesday’s newsletter, we asked you for your opinion on breast vs formula milk (for babies!), and got the above-depicted, below-described, set of responses:
- 80% said “Breast is best, as the slogan goes, and should be first choice”
- 20% said “They both have their strengths and weaknesses; use whatever”
- 0% said “Formula is formulated to be best, and should be first choice”
That’s the first time we’ve ever had a possible poll option come back with zero votes whatsoever! It seems this topic is relatively uncontentious amongst our readership, so we’ll keep things brief today, but there is still a little mythbusting to be done.
So, what does the science say?
[Breast milk should be the first choice] at least for the few few weeks and months for the benefit of baby’s health as breast milk has protective factors formula does not: True or False?
True! The wording here was taken from one of our readers’ responses, by the way (thank you, Robin). There are a good number of those protective factors, the most well-known of which is passing on immune cells and cell-like things; in other words, immune-related information being passed from parent* to child.
*usually the mother, though in principle it could be someone else and in practice sometimes it is; the only real requirements are that the other person be healthy, lactating, and willing.
As for immune benefits, see for example:
Perspectives on Immunoglobulins in Colostrum and Milk
And for that matter, also:
(Colostrum is simply the milk that is produced for a short period after giving birth; the composition of milk will tend to change later)
In any case, immunoglobulin A is a very important component in breast milk (colostrum and later), as well as lactoferrin (has an important antimicrobial effect and is good for the newborn’s gut), and a plethora of cytokines:
As for that about the gut, lactoferrin isn’t the only breast milk component that benefits this, by far, and there’s a lot that can’t be replicated yet:
Human Breast Milk and the Gastrointestinal Innate Immune System
As long as your infant/child is nutritiously fed, it shouldn’t matter if it comes from breast or formula: True or False?
False! Formula milk will not convey those immune benefits.
This doesn’t mean that formula-feeding is neglectful; as several people who commented mentioned*, there are many reasons a person may not be able to breastfeed, and they certainly should not be shamed for that.
*(including the reader whose words we borrowed for this True/False item; the words we quoted above were prefaced with: “Not everyone is able to breastfeed for many different reasons”)
But, while formula milk is a very good second choice, and absolutely a respectable choice if breast milk isn’t an option (or an acceptable option) for whatever reason, it still does not convey all the health benefits of breast milk—yet! The day may come when they’ll find a way to replicate the immune benefits, but today is not that day.
They both have their strengths and weaknesses: True or False?
True! But formula’s strengths are only in the category of convenience and sometimes necessity—formula conveys no health benefits that breast milk could not do better, if available.
For many babies, formula means they get to eat, when without it they would starve due to non-availability of breast milk. That’s a pretty important role!
Note also: this is a health science publication, not a philosophical publication, but we’d be remiss not to mention one thing; let’s bring it in under the umbrella of sociology:
The right to bodily autonomy continues to be the right to bodily autonomy even if somebody else wants/needs something from your body.
Therefore, while there are indeed many good reasons for not being able to breastfeed, or even just not being safely* able to breastfeed, it is at the very least this writer’s opinion that nobody should be pressed to give their reason for not breastfeeding; “no” is already a sufficient answer.
*Writer’s example re safety: when I was born, my mother was on such drugs that it would have been a very bad idea for her to breastfeed me. There are plenty of other possible reasons why it might be unsafe for someone one way or another, but “on drugs that have a clear ‘do not take while pregnant or nursing’ warning” is a relatively common one.
All that said, for those who are willing and safely able, the science is clear: breast is best.
Want to read more?
The World Health Organization has a wealth of information (including explanations of its recommendations of, where possible, exclusive breastfeeding for the first 6 months, ideally continuing some breastfeeding for the first 2 years), here:
World Health Organization | Breastfeeding
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 4 Best Stretches To Do Before Bed (And Even: To Do In Bed!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Contrary to the stereotype of early morning yoga sessions, the evening is actually the best time to improve flexibility.
Not only that, but there are benefits to stretching on a soft surface, such as your bed, rather than the floor—in few words, it reduces the nervous feedback that limits your flexibility.
The most comfortable yoga session
Here are three great stretches to do of an evening:
Frog pose:
- Spread your knees wide, forming 90° angles at your ankles, knees, and hips.
- Press your hips downward and experiment with tilting your tailbone upwards.
- Hold for 1–3 minutes, breathing calmly.
Half straddle stretch:
- This stretch is done with one leg extended, and your other leg bent with foot against your inner thigh.
- Keep your lower back elongated while folding forward.
- Adjust the stretch’s focus by moving towards the middle or towards the extended leg, to stretch your inner thighs more or your hamstrings more, respectively.
- Hold for 1–2 minutes per leg.
Tabletop chest stretch:
- From a tabletop position, walk/slide your hands forward and drop your chest down.
- Hold for at least 1 minute, breathing deeply.
- Variations:
- Turn thumbs upward to engage side muscles.
- Cross arms to stretch the ribs.
Cross-legged forward fold:
- Start in a cross-legged seated position and slightly shift your hips backwards.
- Fold forward, allowing the spine to round.
- Hold for 1–3 minutes, breathing calmly.
This latter is especially good despite its simplicity, as it provides a deep stretch in the outer hips and lower back.
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Over 50? Do These 3 Stretches Every Morning To Avoid Pain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Polyvagal Theory – by Dr. Stephen Porges
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you ever find that your feelings (or occasionally: lack thereof) sometimes can seem mismatched with the observed facts of your situation? This book unravels that mystery—or rather, that stack of mysteries.
Dr. Porges’ work on this topic is, by the way, the culmination of 40 years of research. While he’s not exactly a household name to the layperson, he’s very respected in his field, and this book is his magnum opus.
Here he explains the disparate roles of the two branches of the vagus nerve (hence: polyvagal theory). At least, the two branches that we mammals have; non-mammalian vertebrates have only one. This makes a big difference, because of the cascade of inhibitions that this allows.
The answer to the very general question “What stops you from…?” is usually found somewhere down this line of cascade of inhibitions.
These range from “what stops you from quitting your job/relationship/etc” to “what stops you from freaking out” to “what stops you from relaxing” to “what stops you from reacting quickly” to “what stop you from giving up” to “what stops you from gnawing your arm off” and many many more.
And because sometimes we wish we could do something that we can’t, or wish we wouldn’t do something that we do, understanding this process can be something of a cheat code to life.
A quick note on style: the book is quite dense and can be quite technical, but should be comprehensible to any layperson who is content to take their time, because everything is explained as we go along.
Bottom line: if you’d like to better understand the mysteries of how you feel vs how you actually are, and what that means for what you can or cannot wilfully do, this is a top-tier book
Click here to check out Polyvagal Theory, and take control of your responses!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: