We looked at over 166,000 psychiatric records. Over half showed people were admitted against their will
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Picture two people, both suffering from a serious mental illness requiring hospital admission. One was born in Australia, the other in Asia.
Hopefully, both could be treated on a voluntary basis, taking into account their individual needs, preferences and capacity to consent. If not, you might imagine they should be equally likely to receive treatment against their will (known colloquially as being “sectioned” or “scheduled”).
However, our research published in British Journal of Psychiatry Open suggests this is not the case.
In the largest study globally of its kind, we found Australians are more likely to be treated in hospital for their acute mental illness against their will if they are born overseas, speak a language other than English or are unemployed.
What we did and what we found
We examined more than 166,000 episodes of voluntary and involuntary psychiatric care in New South Wales public hospitals between 2016 and 2021. Most admissions (54%) included at least one day of involuntary care.
Being brought to hospital via legal means, such as by police or via a court order, was strongly linked to involuntary treatment.
While our study does not show why this is the case, it may be due to mental health laws. In NSW, which has similar laws to most jurisdictions in Australia, doctors may treat a person on an involuntary basis if they present with certain symptoms indicating serious mental illness (such as hallucinations and delusions) which cause them to require protection from serious harm, and there is no other less-restrictive care available. Someone who has been brought to hospital by police or the courts may be more likely to meet the legal requirement of requiring protection from serious harm.
The likelihood of involuntary care was also linked to someone’s diagnosis. A person with psychosis or organic brain diseases, such as dementia and delirium, were about four times as likely to be admitted involuntarily compared to someone with anxiety or adjustment disorders (conditions involving a severe reaction to stressors).
However, our data suggest non-clinical factors contribute to the decision to impose involuntary care.
Compared with people born in Australia, we found people born in Asia were 42% more likely to be treated involuntarily.
People born in Africa or the Middle East were 32% more likely to be treated this way.
Overall, people who spoke a language other than English were 11% more likely to receive involuntary treatment compared to those who spoke English as their first language.
Some international researchers have suggested higher rates of involuntary treatment seen in people born overseas might be due to higher rates of psychotic illness. But our research found a link between higher rates of involuntary care in people born overseas or who don’t speak English regardless of their diagnosis.
We don’t know why this is happening. It is likely to reflect a complex interplay of factors about both the people receiving treatment and the way services are provided to them.
People less likely to be treated involuntarily included those who hold private health insurance, and those referred through a community health centre or outpatients unit.
Our findings are in line with international studies. These show higher rates of involuntary treatment among people from Black and ethnic minority groups, and people living in areas of higher socioeconomic disadvantage.
A last resort? Or should we ban it?
Both the NSW and Australian mental health commissions have called involuntary psychiatric care an avoidable harm that should only be used as a last resort.
Despite this, one study found Australia’s rate of involuntary admissions has increased by 3.4% per year and it has one of the highest rates of involuntary admissions in the world.
Involuntary psychiatric treatment is also under increasing scrutiny globally.
When Australia signed up to the UN Convention on the Rights of Persons with Disabilities, it added a declaration noting it would allow for involuntary treatment of people with mental illness where such treatments are “necessary, as a last resort and subject to safeguards”.
However, the UN has rejected this, saying it is a fundamental human right “to be free from involuntary detention in a mental health facility and not to be forced to undergo mental health treatment”.
Others question if involuntary treatment could ever be removed entirely.
Where to from here?
Our research not only highlights concerns regarding how involuntary psychiatric treatment is implemented, it’s a first step towards decreasing its use. Without understanding how and when it is used it will be difficult to create effective interventions to reduce it.
But Australia is still a long way from significantly reducing involuntary treatment.
We need to provide more care options outside hospital, ones accessible to all Australians, including those born overseas, who don’t speak English, or who come from disadvantaged communities. This includes intervening early enough that people are supported to not become so unwell they end up being referred for treatment via police or the criminal justice system.
More broadly, we need to do more to reduce stigma surrounding mental illness and to ensure poverty and discrimination are tackled to help prevent more people becoming unwell in the first place.
Our study also shows we need to do more to respect the autonomy of someone with serious mental illness to choose if they are treated. That’s whether they are in NSW or other jurisdictions.
And legal reform is required to ensure more states and territories more fully reflect the principal that people who have the capacity to make such decisions should have the right to decline mental health treatment in the same way they would any other health care.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Amy Corderoy, Medical doctor and PhD candidate studying involuntary psychiatric treatment, School of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Water Water Everywhere, But Which Is Best To Drink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well Well Well…
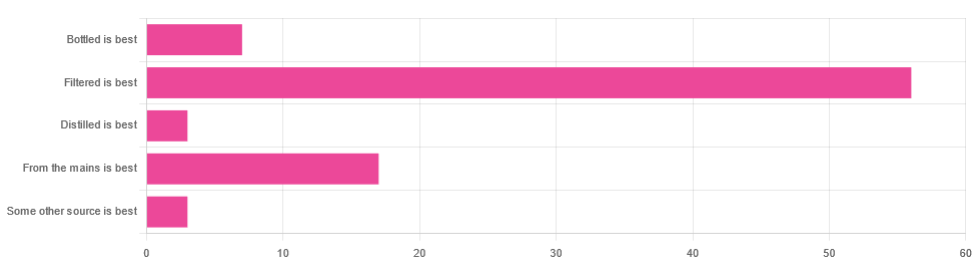
In Tuesday’s newsletter, we asked you for your (health-related) opinion on drinking water—with the understanding that this may vary from place to place. We got the above-depicted, below-described, set of responses:
- About 65% said “Filtered is best”
- About 20% said “From the mains is best”
- About 8% said “Bottled is best”
- About 3% said “Distilled is best”
- About 3% said “Some other source is best”
Of those who said “some other source is best”, one clarified that their preferred source was well water.
So what does the science say?
Fluoridated water is bad for you: True or False?
False, assuming a normal level of consumption. Rather than take up more space today though, we’ll link to what we previously wrote on this topic:
You may be wondering: but what if my level of consumption is higher than normal?
Let’s quickly look at some stats:
- The maximum permitted safety level varies from place to place, but is (for example) 2mg/l in the US, 1.5mg/l in Canada & the UK.
- The minimum recommended amount also varies from place to place, but is (for example) 0.7mg/l in Canada and the US, and 1mg/l in the UK.
It doesn’t take grabbing a calculator to realize that if you drink twice as much water as someone else, then depending on where you are, water fluoridated to the minimum may give you more than the recommended maximum.
However… Those safety margins are set so much lower than the actual toxicity levels of fluoride, that it doesn’t make a difference.
For example: your writer here takes a medication that has the side effect of causing dryness of the mouth, and consequently she drinks at least 3l of water per day in a climate that could not be described as hot (except perhaps for about 2 weeks of the year). She weighs 72kg (that’s about 158 pounds), and the toxicity of fluoride (for ill symptoms, not death) is 0.2mg/kg. So, she’d need 14.4mg of fluoride, which even if the water fluoridation here were 2mg/l (it’s not; it’s lower here, but let’s go with the highest figure to make a point), would require drinking more than 7l of water faster than the body can process it.
For more about the numbers, check out:
Acute Fluoride Poisoning from a Public Water System
Bottled water is the best: True or False?
False, if we consider “best” to be “healthiest”, which in turn we consider to be “most nutrients, with highest safety”.
Bottled water generally does have higher levels of minerals than most local mains supply water does. That’s good!
But you know what else is generally has? Microplastics and nanoplastics. That’s bad!
We don’t like to be alarmist in tone; it’s not what we’re about here, but the stats on bottled water are simply not good; see:
We Are Such Stuff As Bottles Are Made Of
You may be wondering: “but what about bottled water that comes in glass bottles?”
Indeed, water that comes in glass bottles can be expected to have lower levels of plastic than water that comes in plastic bottles, for obvious reasons.
However, we invite you to consider how likely you believe it to be that the water wasn’t stored in plastic while being processed, shipped and stored, before being portioned into its final store-ready glass bottles for end-consumer use.
Distilled water is the best: True or False?
False, generally, with caveats:
Distilled water is surely the safest water anywhere, because you know that you’ve removed any nasties.
However, it’s also devoid of nutrients, because you also removed any minerals it contained. Indeed, if you use a still, you’ll be accustomed to the build-up of these minerals (generally simplified and referenced as “limescale”, but it’s a whole collection of minerals).
Furthermore, that loss of nutrients can be more than just a “something good is missing”, because having removed certain ions, that water could now potentially strip minerals from your teeth. In practice, however, you’d probably have to swill it excessively to cause this damage.
Nevertheless, if you have the misfortune of living somewhere like Flint, Michigan, then a water still may be a fair necessity of life. In other places, it can simply be useful to have in case of emergency, of course.
Here’s an example product on Amazon if you’d like to invest in a water still for such cases.
PS: distilled water is also tasteless, and is generally considered bad, tastewise, for making tea and coffee. So we really don’t recommend distilling your water unless you have a good reason to do so.
Filtered water is the best: True or False?
True for most people in most places.
Let’s put it this way: it can’t logically be worse than whatever source of water you put into it…
Provided you change the filter regularly, of course.
Otherwise, after overusing a filter, at best it won’t be working, and at worst it’ll be adding in bacteria that have multiplied in the filter over however long you left it there.
You may be wondering: can water filters remove microplastics, and can they remove minerals?
The answer in both cases is: sometimes.
- For microplastics it depends on the filter size and the microplastic size (see our previous article for details on that).
- For minerals, it depends on the filter type. Check out:
The H2O Chronicles | 5 Water Filters That Remove Minerals
One other thing to think about: while most water filtration jugs are made of PFAS-free BPA-free plastics for obvious reasons, for greater peace of mind, you might consider investing in a glass filtration jug, like this one ← this is just one example product on Amazon; by all means shop around and find one you like
Take care!
Share This Post
-
For women with antenatal depression, micronutrients might help them and their babies – new study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getty Images Julia J Rucklidge, University of Canterbury; Elena Moltchanova, University of Canterbury; Roger Mulder, University of Otago, and Siobhan A Campbell, University of Canterbury
Antenatal depression affects 15% to 21% of pregnant women worldwide. It can influence birth outcomes and children’s development, as well as increase the risk of post-natal depression.
Current treatments like therapy can be inaccessible and antidepressants can carry risks for developing infants.
Over the past two decades, research has highlighted that poor nutrition is a contributing risk factor to mental health challenges. Most pregnant women in New Zealand aren’t adhering to nutritional guidelines, according to a longitudinal study. Only 3% met the recommendations for all food groups.
Another cohort study carried out in Brazil shows that ultra-processed foods (UPF) accounted for at least 30% of daily dietary energy during pregnancy, displacing healthier options.
UPFs are chemically manufactured and contain additives to improve shelf life, as well as added sugar and salt. Importantly, they are low in essential micronutrients (vitamins and minerals).
The consumption of these foods is concerning because a nutrient-poor diet during pregnancy has been linked to poorer mental health outcomes in children. This includes depression, anxiety, hyperactivity, and inattention.
Increasing nutrients in maternal diets and reducing consumption of UPFs could improve the mental health of the mother and the next generation. Good nutrition can have lifelong benefits for the offspring.
However, there are multiple factors that mean diet change alone may not in itself be sufficient to address mental health challenges. Supplementing with additional nutrients may also be important to address nutritional needs during pregnancy.
Micronutrients as treatment for depression
Our earlier research suggests micronutrient supplements for depression have benefits outside pregnancy.
But until now there have been no published randomised controlled trials specifically designed to assess the efficacy and safety of broad-spectrum micronutrients on antenatal depression and overall functioning.
The NUTRIMUM trial, which ran between 2017 and 2022, recruited 88 women in their second trimester of pregnancy who reported moderate depressive symptoms. They were randomly allocated to receive either 12 capsules (four pills, three times a day) of a broad-spectrum micronutrient supplement or an active placebo containing iodine and riboflavin for a 12-week period.
Micronutrient doses were generally between the recommended dietary allowance and the tolerable upper level.
Based on clinician ratings, micronutrients significantly improved overall psychological functioning compared to the placebo. The findings took into account all noted changes based on self-assessment and clinician observations. This includes sleep, mood regulation, coping, anxiety and side effects.
Adding micronutrients to the diet of pregnant women with antenatal depression significantly improved their overall psychological functioning. Getty Images Both groups reported similar reductions in symptoms of depression. More than three quarters of participants were in remission at the end of the trial. But 69% of participants in the micronutrient group rated themselves as “much” or “very much” improved, compared to 39% in the placebo group.
Participants taking the micronutrients also experienced significantly greater improvements in sleep and overall day-to-day functioning, compared to participants taking the placebo. There were no group differences on measures of stress, anxiety and quality of life.
Importantly, there were no group differences in reported side effects, and reports of suicidal thoughts dropped over the course of the study for both groups. Blood tests confirmed increased vitamin levels (vitamin C, D, B12) and fewer deficiencies in the micronutrient group.
Micronutrients were particularly helpful for women with chronic mental health challenges and those who had taken psychiatric medications in the past. Those with milder symptoms improved with or without the micronutrients, suggesting general care and monitoring might suffice for some women.
The benefits of micronutrients were comparable to psychotherapy but with less contact. There are no randomised controlled trials of antidepressant medication to compare these results.
Retention in the study was good (81%) and compliance excellent (90%).
Beyond maternal mental health
We followed the infants of mothers enrolled in the NUTRIMUM trial (who were therefore exposed to micronutrients during pregnancy) for 12 months, alongside infants from the general population of Aotearoa New Zealand.
This second group of infants from the general population contained a smaller sub-group who were exposed to antidepressant medication for the treatment of antenatal depression.
We assessed the neuro-behavioural development of each infant within the first four weeks of life, and temperament up to one year after birth.
These observational follow-ups showed positive effects of micronutrients on the infants’ ability to regulate their behaviour. These results were on par with or better than typical pregnancies, and better than treatments with antidepressants.
Micronutrients during pregnancy improved the neurological and behavioural development of infants. Getty Images Infants exposed to micronutrients during pregnancy were significantly better at attending to external stimuli. They were also better able to block out external stimuli during sleep. They showed fewer signs of stress and had better muscle tone compared to infants not exposed to micronutrients.
They also displayed greater ability to interact with their environment. They were better at regulating their emotional state and had fewer abnormal muscle reflexes than infants exposed to antidepressant medication in pregnancy.
Reassuringly, micronutrients had no negative impact on infant temperament.
These findings highlight the potential of micronutrients as a safe and effective alternative to traditional medication treatments for antenatal depression.
The prenatal environment sets the foundation for a child’s future. Further investigation into the benefits of micronutrient supplementation would gives us more confidence in their use for other perinatal (from the start of pregnancy to a year after birth) mental health issues. This could provide future generations with a better start to life.
We would like to acknowledge the contribution of Dr Hayley Bradley to this research project.
Julia J Rucklidge, Professor of Psychology, University of Canterbury; Elena Moltchanova, Professor of Statistics, University of Canterbury; Roger Mulder, Professor of Psychiatry, University of Otago, and Siobhan A Campbell, Intern Psychologist, Researcher – Te Puna Toiora (Mental Health and Nutrition Research Lab), University of Canterbury
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Does intermittent fasting increase or decrease our risk of cancer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research over the years has suggested intermittent fasting has the potential to improve our health and reduce the likelihood of developing cancer.
So what should we make of a new study in mice suggesting fasting increases the risk of cancer?
Stock-Asso/Shutterstock What is intermittent fasting?
Intermittent fasting means switching between times of eating and not eating. Unlike traditional diets that focus on what to eat, this approach focuses on when to eat.
There are lots of commonly used intermittent fasting schedules. The 16/8 plan means you only eat within an eight-hour window, then fast for the remaining 16 hours. Another popular option is the 5:2 diet, where you eat normally for five days then restrict calories for two days.
In Australia, poor diet contributes to 7% of all cases of disease, including coronary heart disease, stroke, type 2 diabetes, and cancers of the bowel and lung. Globally, poor diet is linked to 22% of deaths in adults over the age of 25.
Intermittent fasting has gained a lot of attention in recent years for its potential health benefits. Fasting influences metabolism, which is how your body processes food and energy. It can affect how the body absorbs nutrients from food and burns energy from sugar and fat.
What did the new study find?
The new study, published in Nature, found when mice ate again after fasting, their gut stem cells, which help repair the intestine, became more active. The stem cells were better at regenerating compared with those of mice who were either totally fasting or eating normally.
This suggests the body might be better at healing itself when eating after fasting.
However, this could also have a downside. If there are genetic mutations present, the burst of stem cell-driven regeneration after eating again might make it easier for cancer to develop.
Polyamines – small molecules important for cell growth – drive this regeneration after refeeding. These polyamines can be produced by the body, influenced by diet, or come from gut bacteria.
The findings suggest that while fasting and refeeding can improve stem cell function and regeneration, there might be a tradeoff with an increased risk of cancer, especially if fasting and refeeding cycles are repeated over time.
While this has been shown in mice, the link between intermittent fasting and cancer risk in humans is more complicated and not yet fully understood.
What has other research found?
Studies in animals have found intermittent fasting can help with weight loss, improve blood pressure and blood sugar levels, and subsequently reduce the risks of diabetes and heart disease.
Research in humans suggests intermittent fasting can reduce body weight, improve metabolic health, reduce inflammation, and enhance cellular repair processes, which remove damaged cells that could potentially turn cancerous.
However, other studies warn that the benefits of intermittent fasting are the same as what can be achieved through calorie restriction, and that there isn’t enough evidence to confirm it reduces cancer risk in humans.
What about in people with cancer?
In studies of people who have cancer, fasting has been reported to protect against the side effects of chemotherapy and improve the effectiveness of cancer treatments, while decreasing damage to healthy cells.
Prolonged fasting in some patients who have cancer has been shown to be safe and may potentially be able to decrease tumour growth.
On the other hand, some experts advise caution. Studies in mice show intermittent fasting could weaken the immune system and make the body less able to fight infection, potentially leading to worse health outcomes in people who are unwell. However, there is currently no evidence that fasting increases the risk of bacterial infections in humans.
So is it OK to try intermittent fasting?
The current view on intermittent fasting is that it can be beneficial, but experts agree more research is needed. Short-term benefits such as weight loss and better overall health are well supported. But we don’t fully understand the long-term effects, especially when it comes to cancer risk and other immune-related issues.
Since there are many different methods of intermittent fasting and people react to them differently, it’s hard to give advice that works for everyone. And because most people who participated in the studies were overweight, or had diabetes or other health problems, we don’t know how the results apply to the broader population.
For healthy people, intermittent fasting is generally considered safe. But it’s not suitable for everyone, particularly those with certain medical conditions, pregnant or breastfeeding women, and people with a history of eating disorders. So consult your health-care provider before starting any fasting program.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Her Mental Health Treatment Was Helping. That’s Why Insurance Cut Off Her Coverage.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reporting Highlights
- Progress Denials: Insurers use a patient’s improvement to justify denying mental health coverage.
- Providers Disagree: Therapists argue with insurers and the doctors they employ to continue covering treatment for their patients.
- Patient Harm: Some patients backslid when insurers cut off coverage for treatment at key moments.
These highlights were written by the reporters and editors who worked on this story.
Geneva Moore’s therapist pulled out her spiral notebook. At the top of the page, she jotted down the date, Jan. 30, 2024, Moore’s initials and the name of the doctor from the insurance company to whom she’d be making her case.
She had only one chance to persuade him, and by extension Blue Cross and Blue Shield of Texas, to continue covering intensive outpatient care for Moore, a patient she had come to know well over the past few months.
The therapist, who spoke on the condition of anonymity out of fear of retaliation from insurers, spent the next three hours cramming, as if she were studying for a big exam. She combed through Moore’s weekly suicide and depression assessments, group therapy notes and write-ups from their past few sessions together.
She filled two pages with her notes: Moore had suicidal thoughts almost every day and a plan for how she would take her own life. Even though she expressed a desire to stop cutting her wrists, she still did as often as three times a week to feel the release of pain. She only had a small group of family and friends to offer support. And she was just beginning to deal with her grief and trauma over sexual and emotional abuse, but she had no healthy coping skills.
Less than two weeks earlier, the therapist’s supervisor had struck out with another BCBS doctor. During that call, the insurance company psychiatrist concluded Moore had shown enough improvement that she no longer needed intensive treatment. “You have made progress,” the denial letter from BCBS Texas read.
When the therapist finally got on the phone with a second insurance company doctor, she spoke as fast as she could to get across as many of her points as possible.
“The biggest concern was the abnormal thoughts — the suicidal ideation, self-harm urges — and extensive trauma history,” the therapist recalled in an interview with ProPublica. “I was really trying to emphasize that those urges were present, and they were consistent.”
She told the company doctor that if Moore could continue on her treatment plan, she would likely be able to leave the program in 10 weeks. If not, her recovery could be derailed.
The doctor wasn’t convinced. He told the therapist that he would be upholding the initial denial. Internal notes from the BCBS Texas doctors say that Moore exhibited “an absence of suicidal thoughts,” her symptoms had “stabilized” and she could “participate in a lower level of care.”
The call lasted just seven minutes.
Moore was sitting in her car during her lunch break when her therapist called to give her the news. She was shocked and had to pull herself together to resume her shift as a technician at a veterinary clinic.
“The fact that it was effective immediately,” Moore said later, “I think that was the hardest blow of it all.”
Many Americans must rely on insurers when they or family members are in need of higher-touch mental health treatment, such as intensive outpatient programs or round-the-clock care in a residential facility. The costs are high, and the stakes for patients often are, too. In 2019 alone, the U.S. spent more than $106.5 billion treating adults with mental illness, of which private insurance paid about a third. One 2024 study found that the average quoted cost for a month at a residential addiction treatment facility for adolescents was more than $26,000.
Health insurers frequently review patients’ progress to see if they can be moved down to a lower — and almost always cheaper — level of care. That can cut both ways. They sometimes cite a lack of progress as a reason to deny coverage, labeling patients’ conditions as chronic and asserting that they have reached their baseline level of functioning. And if they make progress, which would normally be celebrated, insurers have used that against patients to argue they no longer need the care being provided.
Their doctors are left to walk a tightrope trying to convince insurers that patients are making enough progress to stay in treatment as long as they actually need it, but not so much that the companies prematurely cut them off from care. And when insurers demand that providers spend their time justifying care, it takes them away from their patients.
“The issues that we grapple with are in the real world,” said Dr. Robert Trestman, the chair of psychiatry and behavioral medicine at the Virginia Tech Carilion School of Medicine and chair of the American Psychiatric Association’s Council on Healthcare Systems and Financing. “People are sicker with more complex conditions.”
Mental health care can be particularly prone to these progress-based denials. While certain tests reveal when cancer cells are no longer present and X-rays show when bones have healed, psychiatrists say they have to determine whether someone has returned to a certain level of functioning before they can end or change their treatment. That can be particularly tricky when dealing with mental illness, which can be fluid, with a patient improving slightly one day only to worsen the next.
Though there is no way to know how often coverage gets cut off mid-treatment, ProPublica has found scores of lawsuits over the past decade in which judges have sharply criticized insurance companies for citing a patient’s improvement to deny mental health coverage. In a number of those cases, federal courts ruled that the insurance companies had broken a federal law designed to provide protections for people who get health insurance through their jobs.
Reporters reviewed thousands of pages of court documents and interviewed more than 50 insiders, lawyers, patients and providers. Over and over, people said these denials can lead to real — sometimes devastating — harm. An official at an Illinois facility with intensive mental health programs said that this past year, two patients who left before their clinicians felt they were ready due to insurance denials had attempted suicide.
Dr. Eric Plakun, a Massachusetts psychiatrist with more than 40 years of experience in residential and intensive outpatient programs, and a former board member of the American Psychiatric Association, said the “proprietary standards” insurers use as a basis for denying coverage often simply stabilize patients in crisis and “shortcut real treatment.”
Plakun offered an analogy: If someone’s house is on fire, he said, putting out the fire doesn’t restore the house. “I got a hole in the roof, and the windows have been smashed in, and all the furniture is charred, and nothing’s working electrically,” he said. “How do we achieve recovery? How do we get back to living in that home?”
Unable to pay the $350-a-day out-of-pocket cost for additional intensive outpatient treatment, Moore left her program within a week of BCBS Texas’ denial. The insurer would only cover outpatient talk therapy.
During her final day at the program, records show, Moore’s suicidal thoughts and intent to carry them out had escalated from a 7 to a 10 on a 1-to-10 scale. She was barely eating or sleeping.
A few hours after the session, Moore drove herself to a hospital and was admitted to the emergency room, accelerating a downward spiral that would eventually cost the insurer tens of thousands of dollars, more than the cost of the treatment she initially requested.
How Insurers Justify Denials
Buried in the denial letters that insurance companies send patients are a variety of expressions that convey the same idea: Improvement is a reason to deny coverage.
“You are better.” “Your child has made progress.” “You have improved.”
In one instance, a doctor working for Regence Blue Cross and Blue Shield of Oregon wrote that a patient who had been diagnosed with major depression was “sufficiently stable,” even as her own doctors wrote that she “continued to display a pattern of severe impairment” and needed round-the-clock care. A judge ruled that “a preponderance of the evidence” demonstrated that the teen’s continued residential treatment was medically necessary. The insurer said it can’t comment on the case because it ended with a confidential settlement.
In another, a doctor working for UnitedHealth Group wrote in 2019 that a teenage girl with a history of major depression who had been hospitalized after trying to take her own life by overdosing “was doing better.” The insurer denied ongoing coverage at a residential treatment facility. A judge ruled that the insurer’s determination “lacked any reasoning or citations” from the girl’s medical records and found that the insurer violated federal law. United did not comment on this case but previously argued that the girl no longer had “concerning medical issues” and didn’t need treatment in a 24-hour monitored setting.
To justify denials, the insurers cite guidelines that they use to determine how well a patient is doing and, ultimately, whether to continue paying for care. Companies, including United, have said these guidelines are independent, widely accepted and evidence-based.
Insurers most often turn to two sets: MCG (formerly known as Milliman Care Guidelines), developed by a division of the multibillion-dollar media and information company Hearst, and InterQual, produced by a unit of UnitedHealth’s mental health division, Optum. Insurers have also used guidelines they have developed themselves.
MCG Health did not respond to multiple requests for comment. A spokesperson for the Optum division that works on the InterQual guidelines said that the criteria “is a collection of established scientific evidence and medical practice intended for use as a first level screening tool” and “helps to move patients safely and efficiently through the continuum of care.”
A separate spokesperson for Optum also said the company’s “priority is ensuring the people we serve receive safe and effective care for their individual needs.” A Regence spokesperson said that the company does “not make coverage decisions based on cost or length of stay,” and that its “number one priority is to ensure our members have access to the care they need when they need it.”
In interviews, several current and former insurance employees from multiple companies said that they were required to prioritize the proprietary guidelines their company used, even if their own clinical judgment pointed in the opposite direction.
“It’s very hard when you come up against all these rules that are kind of setting you up to fail the patient,” said Brittainy Lindsey, a licensed mental health counselor who worked at the Anthem subsidiary Beacon and at Humana for a total of six years before leaving the industry in 2022. In her role, Lindsey said, she would suggest approving or denying coverage, which — for the latter — required a staff doctor’s sign-off. She is now a mental health consultant for behavioral health businesses and clinicians.
A spokesperson for Elevance Health, formerly known as Anthem, said Lindsey’s “recollection is inaccurate, both in terms of the processes that were in place when she was a Beacon employee, and how we operate today.” The spokesperson said “clinical judgment by a physician — which Ms. Lindsey was not — always takes precedence over guidelines.”
In an emailed statement, a Humana spokesperson said the company’s clinician reviewers “are essential to evaluating the facts and circumstances of each case.” But, the spokesperson said, “having objective criteria is also important to provide checks and balances and consistently comply with” federal requirements.
The guidelines are a pillar of the health insurance system known as utilization management, which paves the way for coverage denials. The process involves reviewing patients’ cases against relevant criteria every handful of days or so to assess if the company will continue paying for treatment, requiring providers and patients to repeatedly defend the need for ongoing care.
Federal judges have criticized insurance company doctors for using such guidelines in cases where they were not actually relevant to the treatment being requested or for “solely” basing their decisions on them.
Wit v. United Behavioral Health, a class-action lawsuit involving a subsidiary of UnitedHealth, has become one of the most consequential mental health cases of this century. In that case, a federal judge in California concluded that a number of United’s in-house guidelines did not adhere to generally accepted standards of care. The judge found that the guidelines allowed the company to wrongly deny coverage for certain mental health and substance use services the moment patients’ immediate problems improved. He ruled that the insurer would need to change its practices. United appealed the ruling on grounds other than the court’s findings about the defects in its guidelines, and a panel of judges partially upheld the decision. The case has been sent back to the district court for further proceedings.
Largely in response to the Wit case, nine states have passed laws requiring health insurers to use guidelines that align with the leading standards of mental health care, like those developed by nonprofit professional organizations.
Cigna has said that it “has chosen not to adopt private, proprietary medical necessity criteria” like MCG. But, according to a review of lawsuits, denial letters have continued to reference MCG. One federal judge in Utah called out the company, writing that Cigna doctors “reviewed the claims under medical necessity guidelines it had disavowed.” Cigna did not respond to specific questions about this.
Timothy Stock, one of the BCBS doctors who denied Moore’s request to cover ongoing care, had cited MCG guidelines when determining she had improved enough — something judges noted he had done before. In 2016, Stock upheld a decision on appeal to deny continued coverage for a teenage girl who was in residential treatment for major depression, post-traumatic stress disorder and anxiety. Pointing to the guidelines, Stock concluded she had shown enough improvement.
The patient’s family sued the insurer, alleging it had wrongly denied coverage. Blue Cross and Blue Shield of Illinois argued that there was evidence that showed the patient had been improving. But, a federal judge found the insurer misstated its significance. The judge partially ruled in the family’s favor, zeroing in on Stock and another BCBS doctor’s use of improvement to recommend denying additional care.
“The mere incidence of some improvement does not mean treatment was no longer medically necessary,” the Illinois judge wrote.
In another case, BCBS Illinois denied coverage for a girl with a long history of mental illness just a few weeks into her stay at a residential treatment facility, noting that she was “making progressive improvements.” Stock upheld the denial after an appeal.
Less than two weeks after Stock’s decision, court records show, she cut herself on the arm and leg with a broken light bulb. The insurer defended the company’s reasoning by noting that the girl “consistently denied suicidal ideation,” but a judge wrote that medical records show the girl was “not forthcoming” with her doctors about her behaviors. The judge ruled against the insurer, writing that Stock and another BCBS doctor “unreasonably ignored the weight of the medical evidence” showing that the girl required residential treatment.
Stock declined to comment. A spokesperson for BCBS said the company’s doctors who review requests for mental health coverage are board certified psychiatrists with multiple years of practice experience. The spokesperson added that the psychiatrists review all information received “from the provider, program and members to ensure members are receiving benefits for the right care, at the right place and at the right time.”
The BCBS spokesperson did not address specific questions related to Moore or Stock. The spokesperson said that the examples ProPublica asked about “are not indicative of the experience of the vast majority of our members,” and that it is committed to providing “access to quality, cost-effective physical and behavioral health care.”
A Lifelong Struggle
A former contemporary dancer with a bright smile and infectious laugh, Moore’s love of animals is eclipsed only by her affinity for plants. She moved from Indiana to Austin, Texas, about six years ago and started as a receptionist at a clinic before working her way up to technician.
Moore’s depression has been a constant in her life. It began as a child, when, she said, she was sexually and emotionally abused. She was able to manage as she grew up, getting through high school and attending Indiana University. But, she said, she fell back into a deep sadness after she learned in 2022 that the church she found comfort in as a college student turned out to be what she and others deemed a cult. In September of last year, she began an intensive outpatient program, which included multiple group and individual therapy sessions every week.
Moore, 32, had spent much of the past eight months in treatment for severe depression, post-traumatic stress disorder and anxiety when BCBS said it would no longer pay for the program in January.
The denial had come to her without warning.
“I was starting to get to the point where I did have some hope, and I was like, maybe I can see an actual end to this,” Moore said. “And it was just cut off prematurely.”
At the Austin emergency room where she drove herself after her treatment stopped, her heart raced. She was given medication as a sedative for her anxiety. According to hospital records she provided to ProPublica, Moore’s symptoms were brought on after “insurance said they would no longer pay.”
A hospital social worker frantically tried to get her back into the intensive outpatient program.
“That’s the sad thing,” said Kandyce Walker, the program’s director of nursing and chief operating officer, who initially argued Moore’s case with BCBS Texas. “To have her go from doing a little bit better to ‘I’m going to kill myself.’ It is so frustrating, and it’s heartbreaking.”
After the denial and her brief admission to the hospital emergency department in January, Moore began slicing her wrists more frequently, sometimes twice a day. She began to down six to seven glasses of wine a night.
“I really had thought and hoped that with the amount of work I’d put in, that I at least would have had some fumes to run on,” she said.
She felt embarrassed when she realized she had nothing to show for months of treatment. The skills she’d just begun to practice seemed to disappear under the weight of her despair. She considered going into debt to cover the cost of ongoing treatment but began to think that she’d rather end her life.
“In my mind,” she said, “that was the most practical thing to do.”
Whenever the thought crossed her mind — and it usually did multiple times a day — she remembered that she had promised her therapist that she wouldn’t.
Moore’s therapist encouraged her to continue calling BCBS Texas to try to restore coverage for more intensive treatment. In late February, about five weeks after Stock’s denial, records show that the company approved a request that sent her back to the same facility and at the same level of care as before.
But by that time, her condition had deteriorated so severely that it wasn’t enough.
Eight days later, Moore was admitted to a psychiatric hospital about half an hour from Austin. Medical records paint a harrowing picture of her condition. She had a plan to overdose and the medicine to do it. The doctor wrote that she required monitoring and had “substantial ongoing suicidality.” The denial continued to torment her. She told her doctor that her condition worsened after “insurance stopped covering” her treatment.
Her few weeks stay at the psychiatric hospital cost $38,945.06. The remaining 10 weeks of treatment at the intensive outpatient program — the treatment BCBS denied — would have cost about $10,000.
Moore was discharged from the hospital in March and went back into the program Stock had initially said she no longer needed.
It marked the third time she was admitted to the intensive outpatient program.
A few months later, as Moore picked at her lunch, her oversized glasses sliding down the bridge of her nose every so often, she wrestled with another painful realization. Had the BCBS doctors not issued the denial, she probably would have completed her treatment by now.
“I was really looking forward to that,” Moore said softly. As she spoke, she played with the thick stack of bracelets hiding the scars on her wrists.
A few weeks later, that small facility closed in part because of delays and denials from insurance companies, according to staff and billing records. Moore found herself calling around to treatment facilities to see which ones would accept her insurance. She finally found one, but in October, her depression had become so severe that she needed to be stepped up to a higher level of care.
Moore was able to get a leave of absence from work to attend treatment, which she worried would affect the promotion she had been working toward. To tide her over until she could go back to work, she used up the money her mother sent for her 30th birthday.
She smiles less than she did even a few months ago. When her roommates ask her to hang out downstairs, she usually declines. She has taken some steps forward, though. She stopped drinking and cutting her wrists, allowing scar tissue to cover her wounds.
But she’s still grieving what the denial took from her.
“I believed I could get better,” she said recently, her voice shaking. “With just a little more time, I could discharge, and I could live life finally.”
Kirsten Berg contributed research.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nonverbal Epiphany – by Dr. Stephen Furlich
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle of this book, “Steps To Improve Your Nonverbal Communication” suggests that this is principally an instructional book—it’s not. Rather, it’s mostly informational, and it is left to the reader to interpret what to do with that information.
But, what a lot of information!
And well-sourced, too: this book has scientific paper citations at a rate of one or two per page, with many diagrams and infographics too. It is, in effect, a treasure trove of physiological, psychological, and sociological data when it comes to nonverbal communication and the various factors that influence it.
So, what can you hope to gain from this book? A lot of sorting out of science vs suppositions, mostly.
From digit ratios to crossed arms, from eye-contact to attire, do things really mean what we’ve been told they mean?
And if they don’t, will people perceive them that way anyway, or will textbook rules go out the window in a real conversation? How about in real nonverbal interactions?
(What’s a nonverbal interaction? It’s the behavior exhibited between strangers in the street, it’s the impression given and received by your profile picture, things like that).
Bottom line is that this book is data, data, and more data. If ever you wanted to sort the psychology from the pseudoscience, this is the book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coca-Cola vs Diet Coke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Coca-Cola to Diet Coke, we picked the Diet Coke.
Why?
While the Diet Coke is bad, the Coca-Cola has mostly the same problems plus sugar.
The sugar in a can of Coca-Cola is 39g high-fructose corn syrup (the worst kind of sugar yet known to humanity), and of course it’s being delivered in liquid form (the most bioavailable way to get, which in this case, is bad).
To put those 39g into perspective, the daily recommended amount of sugar is 36g for men or 25g for women, according to the AHA.
The sweetener in Diet Coke is aspartame, which has had a lot of health risk accusations made against it, most of which have not stood up to scrutiny, and the main risk it does have is “it mimics sugar too well” and it can increase cravings for sweetness, and therefore higher consumption of sugars in other products. For this reason, the World Health Organization has recommended to simply reduce sugar intake without looking to artificial sweeteners to help.
Nevertheless, aspartame has been found safe (in moderate doses; the upper tolerance level would equate to more than 20 cans of diet coke per day) by food safety agencies ranging from the FDA to the EFSA, based on a large body of science.
Other problems that Diet Coke has are present in Coca-Cola too, such as its acidic nature (bad for tooth enamel) and gassy nature (messes with leptin/ghrelin balance).
Summary: the Diet Coke is relatively less unhealthy, but is still bad in numerous ways, and remains best avoided.
Read more:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: