Drug Metabolism (When You’re Not Average!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Your Medications Run Out… Of You
Everybody knows that alcohol can affect medications’ effects, but what of smoking, and what of obesity? And how does the alcohol thing work anyway?
It’s all about the enzymes
Medicines that are processed by the liver (which is: most medicines) are metabolized there by specialist enzymes, and the things we do can increase or decrease the quantity of those enzymes—and/or how active they are.
Dr. Kata Wolff Pederson and her team of researchers at Aarhus University in Denmark examined the livers of recently deceased donors in ways that can’t (ethically) be done with live patients, and were able to find the associations between various lifestyle factors and different levels of enzymes responsible for drug metabolism.
And it’s not always how you might think!
Some key things they found:
- Smokers have twice as high levels of enzyme CYP1A2 than non-smokers, which results in the faster metabolism of a lot of drugs.
- Drinkers have 30% higher levels of enzyme CYP2E1, which also results in a faster metabolism of a lot of drugs.
- Patients with obesity have 50% lower levels of enzyme CYP3A4, resulting in slower metabolism of many drugs
This gets particularly relevant when we take into account the next fact:
- Of the individuals in the study, 40% died from poisoning from a mixture of drugs (usually: prescription and otherwise)
Read in full: Sex- and Lifestyle-Related Factors are Associated with Altered Hepatic CYP Protein Levels
Read a pop-sci article about it: Your lifestyle can determine how well your medicine will work
How much does the metabolism speed matter?
It can matter a lot! If you’re taking drugs and carefully abiding by the dosage instructions, those instructions were assuming they know your speed of metabolism, and this is based on an average.
- If your metabolism is faster, you can get too much of a drug too quickly, and it can harm you
- If your metabolism is faster, it also means that while yes it’ll start working sooner, it’ll also stop working sooner
- If it’s a painkiller, that’s inconvenient. If it’s a drug that keeps you alive, then well, that’s especially unfortunate.
- If your metabolism is slower, it can mean your body is still processing the previous dose(s) when you take the next one, and you can overdose (and potentially die)
We touched on this previously when we talked about obesity in health care settings, and how people can end up getting worse care:
As for alcohol and drugs? Obviously we do not recommend, but here’s some of the science of it with many examples:
Why it’s a bad idea to mix alcohol with some medications
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s may have once spread from person to person, but the risk of that happening today is incredibly low
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
An article published this week in the prestigious journal Nature Medicine documents what is believed to be the first evidence that Alzheimer’s disease can be transmitted from person to person.
The finding arose from long-term follow up of patients who received human growth hormone (hGH) that was taken from brain tissue of deceased donors.
Preparations of donated hGH were used in medicine to treat a variety of conditions from 1959 onwards – including in Australia from the mid 60s.
The practice stopped in 1985 when it was discovered around 200 patients worldwide who had received these donations went on to develop Creuztfeldt-Jakob disease (CJD), which causes a rapidly progressive dementia. This is an otherwise extremely rare condition, affecting roughly one person in a million.
What’s CJD got to do with Alzehimer’s?
CJD is caused by prions: infective particles that are neither bacterial or viral, but consist of abnormally folded proteins that can be transmitted from cell to cell.
Other prion diseases include kuru, a dementia seen in New Guinea tribespeople caused by eating human tissue, scrapie (a disease of sheep) and variant CJD or bovine spongiform encephalopathy, otherwise known as mad cow disease. This raised public health concerns over the eating of beef products in the United Kingdom in the 1980s.
Human growth hormone used to come from donated organs
Human growth hormone (hGH) is produced in the brain by the pituitary gland. Treatments were originally prepared from purified human pituitary tissue.
But because the amount of hGH contained in a single gland is extremely small, any single dose given to any one patient could contain material from around 16,000 donated glands.
An average course of hGH treatment lasts around four years, so the chances of receiving contaminated material – even for a very rare condition such as CJD – became quite high for such people.
hGH is now manufactured synthetically in a laboratory, rather than from human tissue. So this particular mode of CJD transmission is no longer a risk.
Human growth hormone is now produced in a lab.
National Cancer Institute/UnsplashWhat are the latest findings about Alzheimer’s disease?
The Nature Medicine paper provides the first evidence that transmission of Alzheimer’s disease can occur via human-to-human transmission.
The authors examined the outcomes of people who received donated hGH until 1985. They found five such recipients had developed early-onset Alzheimer’s disease.
They considered other explanations for the findings but concluded donated hGH was the likely cause.
Given Alzheimer’s disease is a much more common illness than CJD, the authors presume those who received donated hGH before 1985 may be at higher risk of developing Alzheimer’s disease.
Alzheimer’s disease is caused by presence of two abnormally folded proteins: amyloid and tau. There is increasing evidence these proteins spread in the brain in a similar way to prion diseases. So the mode of transmission the authors propose is certainly plausible.
However, given the amyloid protein deposits in the brain at least 20 years before clinical Alzheimer’s disease develops, there is likely to be a considerable time lag before cases that might arise from the receipt of donated hGH become evident.
When was this process used in Australia?
In Australia, donated pituitary material was used from 1967 to 1985 to treat people with short stature and infertility.
More than 2,000 people received such treatment. Four developed CJD, the last case identified in 1991. All four cases were likely linked to a single contaminated batch.
The risks of any other cases of CJD developing now in pituitary material recipients, so long after the occurrence of the last identified case in Australia, are considered to be incredibly small.
Early-onset Alzheimer’s disease (defined as occurring before the age of 65) is uncommon, accounting for around 5% of all cases. Below the age of 50 it’s rare and likely to have a genetic contribution.
Early onset Alzheimer’s means it occurs before age 65.
perfectlab/ShutterstockThe risk is very low – and you can’t ‘catch’ it like a virus
The Nature Medicine paper identified five cases which were diagnosed in people aged 38 to 55. This is more than could be expected by chance, but still very low in comparison to the total number of patients treated worldwide.
Although the long “incubation period” of Alzheimer’s disease may mean more similar cases may be identified in the future, the absolute risk remains very low. The main scientific interest of the article lies in the fact it’s first to demonstrate that Alzheimer’s disease can be transmitted from person to person in a similar way to prion diseases, rather than in any public health risk.
The authors were keen to emphasise, as I will, that Alzheimer’s cannot be contracted via contact with or providing care to people with Alzheimer’s disease.
Steve Macfarlane, Head of Clinical Services, Dementia Support Australia, & Associate Professor of Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Which gut drugs might end up in a lawsuit? Are there really links with cancer and kidney disease? Should I stop taking them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Common medicines used to treat conditions including heartburn, reflux, indigestion and stomach ulcers may be the subject of a class action lawsuit in Australia.
Lawyers are exploring whether long-term use of these over-the-counter and prescription drugs are linked to stomach cancer or kidney disease.
The potential class action follows the settlement of a related multi-million dollar lawsuit in the United States. Last year, international pharmaceutical company AstraZeneca settled for US$425 million (A$637 million) after patients made the case that two of its drugs caused significant and potentially life-threatening side effects.
Specifically, patients claimed the company’s drugs Nexium (esomeprazole) and Prilosec (omeprazole) increased the risk of kidney damage.
Doucefleur/Shutterstock Which drugs are involved in Australia?
The class of drugs we’re talking about are “proton pump inhibitors” (sometimes called PPIs). In the case of the Australian potential class action, lawyers are investigating:
- Nexium (esomeprazole)
- Losec, Asimax (omeprazole)
- Somac (pantoprazole)
- Pariet (rabeprazole)
- Zoton (lansoprazole).
Depending on their strength and quantity, these medicines are available over-the-counter in pharmacies or by prescription.
They have been available in Australia for more than 20 years and are in the top ten medicines dispensed through the Pharmaceutical Benefits Scheme.
They are used to treat conditions exacerbated by stomach acid. These include heartburn, gastric reflux and indigestion. They work by blocking the protein responsible for pumping acid into the stomach.
These drugs are also prescribed with antibiotics to treat the bacterium Helicobacter pylori, which causes stomach ulcers and stomach cancer.
This class of drugs is also used with antibiotics to treat Helicobacter pylori infections. nobeastsofierce/Shutterstock What do we know about the risks?
Appropriate use of proton pump inhibitors plays an important role in treating several serious digestive problems. Like all medicines, there are risks associated with their use depending on how much and how long they are used.
When proton pump inhibitors are used appropriately for the short-term treatment of stomach problems, they are generally well tolerated, safe and effective.
Their risks are mostly associated with long-term use (using them for more than a year) due to the negative effects from having reduced levels of stomach acid. In elderly people, these include an increased risk of gut and respiratory tract infections, nutrient deficiencies and fractures. Long-term use of these drugs in elderly people has also been associated with an increased risk of dementia.
In children, there is an increased risk of serious infection associated with using these drugs, regardless of how long they are used.
How about the cancer and kidney risk?
Currently, the Australian consumer medicine information sheets that come with the medicines, like this one for esomeprazole, do not list stomach cancer or kidney injury as a risk associated with using proton pump inhibitors.
So what does the evidence say about the risk?
Over the past few years, there have been large studies based on observing people in the general population who have used proton pump inhibitors. These studies have found people who take them are almost two times more likely to develop stomach cancer and 1.7 times more likely to develop chronic kidney disease when compared with people who are not taking them.
In particular, these studies report that users of the drugs lansoprazole and pantoprazole have about a three to four times higher risk than non-users of developing chronic kidney disease.
While these observational studies show a link between using the drugs and these outcomes, we cannot say from this evidence that one causes the other.
Researchers have not yet shown these drugs cause kidney disease. crystal light/Shutterstock What can I do if I’m worried?
Several digestive conditions, especially reflux and heartburn, may benefit from simple dietary and lifestyle changes. But the overall evidence for these is not strong and how well they work varies between individuals.
But it may help to avoid large meals within two to three hours before bed, and reduce your intake of fatty food, alcohol and coffee. Eating slowly and getting your weight down if you are overweight may also help your symptoms.
There are also medications other than proton pump inhibitors that can be used for heartburn, reflux and stomach ulcers.
These include over-the-counter antacids (such as Gaviscon and Mylanta), which work by neutralising the acidic environment of the stomach.
Alternatives for prescription drugs include nizatidine and famotidine. These work by blocking histamine receptors in the stomach, which decreases stomach acid production.
If you are concerned about your use of proton pump inhibitors it is important to speak with your doctor or pharmacist before you stop using them. That’s because when you have been using them for a while, stopping them may result in increased or “rebound” acid production.
Nial Wheate, Professor and Director – Academic Excellence, Macquarie University; Joanna Harnett, Senior Lecturer – Sydney Pharmacy School, Faculty of Medicine and Health, University of Sydney, and Wai-Jo Jocelin Chan, Pharmacist and Associate Lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
“I Stretched Every Day For 30 Days: Game Changer!”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How much can an unflexible person really improve in just 20 minutes per day for a month? Makari Espe finds out:
Consistency really is key
We’re supposed to stretch at least 3 times per week; for many people, the reality is often more like 2 times per year (often the 1st and 2nd of January).
So, how quickly can such neglect be turned around?
Upon initial testing, she found she was even less flexible than thought, and set about her work:
The stretches she used were from random 20-minute full body stretch videos on YouTube, of which there are many, but she used a different one each day. As she went along, she found some favorite kinds of stretching and some favorite instructors, and settled on mostly Peloton stretching videos—she also switched to evening stretching sessions instead of morning.
Along the way, she already noticed gradual improvement in mobility and reduced body tension, and after 3 weeks, it had become a habit that she started craving.
The final test? There’s a marked improvement; see the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Yoga Teacher: “If I wanted to get flexible in 2025, here’s what I’d do”
Take care!
Share This Post
Related Posts
-
Does intermittent fasting have benefits for our brain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intermittent fasting has become a popular dietary approach to help people lose or manage their weight. It has also been promoted as a way to reset metabolism, control chronic disease, slow ageing and improve overall health.
Meanwhile, some research suggests intermittent fasting may offer a different way for the brain to access energy and provide protection against neurodegenerative diseases like Alzheimer’s disease.
This is not a new idea – the ancient Greeks believed fasting enhanced thinking. But what does the modern-day evidence say?
First, what is intermittent fasting?
Our diets – including calories consumed, macronutrient composition (the ratios of fats, protein and carbohydrates we eat) and when meals are consumed – are factors in our lifestyle we can change. People do this for cultural reasons, desired weight loss or potential health gains.
Intermittent fasting consists of short periods of calorie (energy) restriction where food intake is limited for 12 to 48 hours (usually 12 to 16 hours per day), followed by periods of normal food intake. The intermittent component means a re-occurrence of the pattern rather than a “one off” fast.
Food deprivation beyond 24 hours typically constitutes starvation. This is distinct from fasting due to its specific and potentially harmful biochemical alterations and nutrient deficiencies if continued for long periods.
4 ways fasting works and how it might affect the brain
The brain accounts for about 20% of the body’s energy consumption.
Here are four ways intermittent fasting can act on the body which could help explain its potential effects on the brain.
1. Ketosis
The goal of many intermittent fasting routines is to flip a “metabolic switch” to go from burning predominately carbohydrates to burning fat. This is called ketosis and typically occurs after 12–16 hours of fasting, when liver and glycogen stores are depleted. Ketones – chemicals produced by this metabolic process – become the preferred energy source for the brain.
Due to this being a slower metabolic process to produce energy and potential for lowering blood sugar levels, ketosis can cause symptoms of hunger, fatigue, nausea, low mood, irritability, constipation, headaches, and brain “fog”.
At the same time, as glucose metabolism in the brain declines with ageing, studies have shown ketones could provide an alternative energy source to preserve brain function and prevent age-related neurodegeneration disorders and cognitive decline.
Consistent with this, increasing ketones through supplementation or diet has been shown to improve cognition in adults with mild cognitive decline and those at risk of Alzheimer’s disease respectively.
2. Circadian syncing
Eating at times that don’t match our body’s natural daily rhythms can disrupt how our organs work. Studies in shift workers have suggested this might also make us more prone to chronic disease.
Time-restricted eating is when you eat your meals within a six to ten-hour window during the day when you’re most active. Time-restricted eating causes changes in expression of genes in tissue and helps the body during rest and activity.
A 2021 study of 883 adults in Italy indicated those who restricted their food intake to ten hours a day were less likely to have cognitive impairment compared to those eating without time restrictions.
Matching your eating to the active parts of your day may have brain benefits.
Shutterstock3. Mitochondria
Intermittent fasting may provide brain protection through improving mitochondrial function, metabolism and reducing oxidants.
Mitochondria’s main role is to produce energy and they are crucial to brain health. Many age-related diseases are closely related to an energy supply and demand imbalance, likely attributed to mitochondrial dysfunction during ageing.
Rodent studies suggest alternate day fasting or reducing calories by up to 40% might protect or improve brain mitochondrial function. But not all studies support this theory.
4. The gut-brain axis
The gut and the brain communicate with each other via the body’s nervous systems. The brain can influence how the gut feels (think about how you get “butterflies” in your tummy when nervous) and the gut can affect mood, cognition and mental health.
In mice, intermittent fasting has shown promise for improving brain health by increasing survival and formation of neurons (nerve cells) in the hippocampus brain region, which is involved in memory, learning and emotion.
What we eat can affect our brain, and vice versa.
ShutterstockThere’s no clear evidence on the effects of intermittent fasting on cognition in healthy adults. However one 2022 study interviewed 411 older adults and found lower meal frequency (less than three meals a day) was associated with reduced evidence of Alzheimer’s disease on brain imaging.
Some research has suggested calorie restriction may have a protective effect against Alzheimer’s disease by reducing oxidative stress and inflammation and promoting vascular health.
When we look at the effects of overall energy restriction (rather than intermittent fasting specifically) the evidence is mixed. Among people with mild cognitive impairment, one study showed cognitive improvement when participants followed a calorie restricted diet for 12 months.
Another study found a 25% calorie restriction was associated with slightly improved working memory in healthy adults. But a recent study, which looked at the impact of calorie restriction on spatial working memory, found no significant effect.
Bottom line
Studies in mice support a role for intermittent fasting in improving brain health and ageing, but few studies in humans exist, and the evidence we have is mixed.
Rapid weight loss associated with calorie restriction and intermittent fasting can lead to nutrient deficiencies, muscle loss, and decreased immune function, particularly in older adults whose nutritional needs may be higher.
Further, prolonged fasting or severe calorie restriction may pose risks such as fatigue, dizziness, and electrolyte imbalances, which could exacerbate existing health conditions.
If you’re considering intermittent fasting, it’s best to seek advice from a health professional such as a dietitian who can provide guidance on structuring fasting periods, meal timing, and nutrient intake. This ensures intermittent fasting is approached in a safe, sustainable way, tailored to individual needs and goals.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why do some people’s hair and nails grow quicker than mine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout recorded history, our hair and nails played an important role in signifying who we are and our social status. You could say, they separate the caveman from businessman.
It was no surprise then that many of us found a new level of appreciation for our hairdressers and nail artists during the COVID lockdowns. Even Taylor Swift reported she cut her own hair during lockdown.
So, what would happen if all this hair and nail grooming got too much for us and we decided to give it all up. Would our hair and nails just keep on growing?
The answer is yes. The hair on our head grows, on average, 1 centimeter per month, while our fingernails grow an average of just over 3 millimetres.
When left unchecked, our hair and nails can grow to impressive lengths. Aliia Nasyrova, known as the Ukrainian Rapunzel, holds the world record for the longest locks on a living woman, which measure an impressive 257.33 cm.
When it comes to record-breaking fingernails, Diana Armstrong from the United States holds that record at 1,306.58 cm.
Most of us, however, get regular haircuts and trim our nails – some with greater frequency than others. So why do some people’s hair and nails grow more quickly?
Jari Lobo/Pexels Remind me, what are they made out of?
Hair and nails are made mostly from keratin. Both grow from matrix cells below the skin and grow through different patterns of cell division.
Nails grow steadily from the matrix cells, which sit under the skin at the base of the nail. These cells divide, pushing the older cells forward. As they grow, the new cells slide along the nail bed – the flat area under the fingernail which looks pink because of its rich blood supply.
Nails, like hair, are made mostly of keratin. Scott Gruber/Unsplash A hair also starts growing from the matrix cells, eventually forming the visible part of the hair – the shaft. The hair shaft grows from a root that sits under the skin and is wrapped in a sac known as the hair follicle.
This sac has a nerve supply (which is why it hurts to pull out a hair), oil-producing glands that lubricate the hair and a tiny muscle that makes your hair stand up when it’s cold.
At the follicle’s base is the hair bulb, which contains the all-important hair papilla that supplies blood to the follicle.
Matrix cells near the papilla divide to produce new hair cells, which then harden and form the hair shaft. As the new hair cells are made, the hair is pushed up above the skin and the hair grows.
But the papilla also plays an integral part in regulating hair growth cycles, as it sends signals to the stem cells to move to the base of the follicle and form a hair matrix. Matrix cells then get signals to divide and start a new growth phase.
Unlike nails, our hair grows in cycles
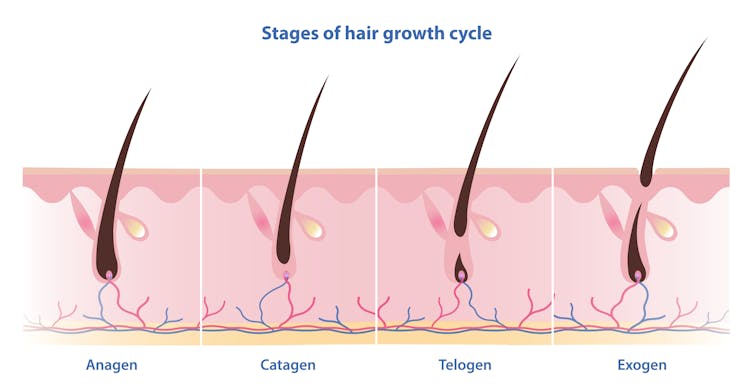
Scientists have identified four phases of hair growth, the:
- anagen or growth phase, which lasts between two and eight years
- catagen or transition phase, when growth slows down, lasting around two weeks
- telogen or resting phase, when there is no growth at all. This usually lasts two to three months
- exogen or shedding phase, when the hair falls out and is replaced by the new hair growing from the same follicle. This starts the process all over again.
Hair follicles enter these phases at different times so we’re not left bald. Mosterpiece/Shutterstock Each follicle goes through this cycle 10–30 times in its lifespan.
If all of our hair follicles grew at the same rate and entered the same phases simultaneously, there would be times when we would all be bald. That doesn’t usually happen: at any given time, only one in ten hairs is in the resting phase.
While we lose about 100–150 hairs daily, the average person has 100,000 hairs on their head, so we barely notice this natural shedding.
So what affects the speed of growth?
Genetics is the most significant factor. While hair growth rates vary between individuals, they tend to be consistent among family members.
Nails are also influenced by genetics, as siblings, especially identical twins, tend to have similar nail growth rates.
Genetics have the biggest impact on growth speed. Cottonbro Studio/Pexels But there are also other influences.
Age makes a difference to hair and nail growth, even in healthy people. Younger people generally have faster growth rates because of the slowing metabolism and cell division that comes with ageing.
Hormonal changes can have an impact. Pregnancy often accelerates hair and nail growth rates, while menopause and high levels of the stress hormone cortisol can slow growth rates.
Nutrition also changes hair and nail strength and growth rate. While hair and nails are made mostly of keratin, they also contain water, fats and various minerals. As hair and nails keep growing, these minerals need to be replaced.
That’s why a balanced diet that includes sufficient nutrients to support your hair and nails is essential for maintaining their health.
Nutrition can impact hair and nail growth. Cottonbro Studio/Pexels Nutrient deficiencies may contribute to hair loss and nail breakage by disrupting their growth cycle or weakening their structure. Iron and zinc deficiencies, for example, have both been linked to hair loss and brittle nails.
This may explain why thick hair and strong, well-groomed nails have long been associated with perception of good health and high status.
However, not all perceptions are true.
No, hair and nails don’t grow after death
A persistent myth that may relate to the legends of vampires is that hair and nails continue to grow after we die.
In reality, they only appear to do so. As the body dehydrates after death, the skin shrinks, making hair and nails seem longer.
Morticians are well aware of this phenomenon and some inject tissue filler into the deceased’s fingertips to minimise this effect.
So, it seems that living or dead, there is no escape from the never-ending task of caring for our hair and nails.
Michelle Moscova, Adjunct Associate Professor, Anatomy, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antibiotics? Think Thrice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antibiotics: Useful Even Less Often Than Previously Believed (And Still Just As Dangerous)
You probably already know that antibiotics shouldn’t be taken unless absolutely necessary. Not only does taking antibiotics frivolously increase antibiotic resistance (which is bad, and kills people), but also…
It’s entirely possible for the antibiotics to not only not help, but instead wipe out your gut’s “good bacteria” that were keeping other things in check.
Those “other things” can include fungi like Candida albicans.
Candida, which we all have in us to some degree, feeds on sugar (including the sugar formed from breaking down alcohol, by the way) and refined carbs. Then it grows, and puts its roots through your intestinal walls, linking with your neural system. Then it makes you crave the very things that will feed it and allow it to put bigger holes in your intestinal walls.
Don’t believe us? Read: Candida albicans-Induced Epithelial Damage Mediates Translocation through Intestinal Barriers
(That’s scientist-speak for “Candida puts holes in your intestines, and stuff can then go through those holes”)
And as for how that comes about, it’s like we said:
See also: Candida albicans as a commensal and opportunistic pathogen in the intestine
That’s not all…
And that’s just C. albicans, never mind things like C. diff. that can just outright kill you easily.
We don’t have room to go into everything here, but you might like to check out:
Four Ways Antibiotics Can Kill You
It gets worse (now comes the new news)
So, what are antibiotics good for? Surely, for clearing up chesty coughs, lower respiratory tract infections, right? It’s certainly one of the two things that antibiotics are most well-known for being good at and often necessary for (the other being preventing/treating sepsis, for example in serious and messy wounds).
But wait…
A large, nationwide (US) observational study of people who sought treatment in primary or urgent care settings for lower respiratory tract infections found…
(drumroll please)
…the use of antibiotics provided no measurable impact on the severity or duration of coughs even if a bacterial infection was present.
Read for yourself:
And in the words of the lead author of that study,
❝Lower respiratory tract infections tend to have the potential to be more dangerous, since about 3% to 5% of these patients have pneumonia. But not everyone has easy access at an initial visit to an X-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection.❞
So, what’s to be done about this? On a large scale, Dr. Merenstein recommends:
❝Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012.❞
This does remind us that, while not a RCT, there is a good ongoing observational study that everyone with a smartphone can participate in:
Dr. Peter Small’s medical AI: “The Cough Doctor”
In the meantime, he advises that when COVID and SARS have been ruled out, then “basic symptom-relieving medications plus time brings a resolution to most people’s infections”.
You can read a lot more detail here:
Antibiotics aren’t effective for most lower tract respiratory infections
In summary…
Sometimes, antibiotics really are a necessary and life-saving medication. But most of the time they’re not, and given their great potential for harm, they may be best simultaneously viewed as the very dangerous threat they also are, and used only when those “heavy guns” are truly what’s required.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: