90% Of People Skip This Essential Exercise—Are You One Of Them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Single-leg strengthening is essential for joint health at any age (unless you want to bunny-hop up and down the stairs with both feet at once, for example), yet many people overlook it. This neglect often leads to pain, stiffness, and a higher risk of injury.
Dr. Alyssa Kuhn, arthritis specialist, explains how to do it:
On the rise
In this video, different exercise variations—beginner, intermediate, and advanced—are presented to help you build strength at your own pace:
Beginner: start by using a chair, adding a cushion for support if needed. Sit at the edge and position one foot slightly in front of the other in a staggered stance. Stand up and sit down in a controlled manner, allowing the back leg to bear more weight and work harder than the front leg. Do 8–10 repetitions per side and pay attention to whether one side feels weaker. To build strength, incorporate this movement into daily activities, such as standing up from the couch. Master this variation before progressing, to avoid knee injury.
Intermediate: to make the exercise more challenging, you can either use a lower chair, or extend your front foot further out, shifting more weight to your back leg. Only modify one variable at a time to maintain control. Do 8–10 repetitions per side, ensuring proper form. A common mistake is allowing the back knee to move inward, which can cause knee stress. To prevent this, use a mirror to check your form and keep the knee and ankle aligned during movement.
Advanced: when you’re ready, extend your front leg completely with the heel on the ground and toes up, removing its stability and forcing the back leg to work even harder. Maintain controlled movement while keeping your knee and ankle aligned. Repeat the exercise on both sides, focusing extra effort on the weaker leg to build balanced strength.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can Medical Schools Funnel More Doctors Into the Primary Care Pipeline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout her childhood, Julia Lo Cascio dreamed of becoming a pediatrician. So, when applying to medical school, she was thrilled to discover a new, small school founded specifically to train primary care doctors: NYU Grossman Long Island School of Medicine.
Now in her final year at the Mineola, New York, school, Lo Cascio remains committed to primary care pediatrics. But many young doctors choose otherwise as they leave medical school for their residencies. In 2024, 252 of the nation’s 3,139 pediatric residency slots went unfilled and family medicine programs faced 636 vacant residencies out of 5,231 as students chased higher-paying specialties.
Lo Cascio, 24, said her three-year accelerated program nurtured her goal of becoming a pediatrician. Could other medical schools do more to promote primary care? The question could not be more urgent. The Association of American Medical Colleges projects a shortage of 20,200 to 40,400 primary care doctors by 2036. This means many Americans will lose out on the benefits of primary care, which research shows improves health, leading to fewer hospital visits and less chronic illness.
Many medical students start out expressing interest in primary care. Then they end up at schools based in academic medical centers, where students become enthralled by complex cases in hospitals, while witnessing little primary care.
The driving force is often money, said Andrew Bazemore, a physician and a senior vice president at the American Board of Family Medicine. “Subspecialties tend to generate a lot of wealth, not only for the individual specialists, but for the whole system in the hospital,” he said.
A department’s cache of federal and pharmaceutical-company grants often determines its size and prestige, he said. And at least 12 medical schools, including Harvard, Yale, and Johns Hopkins, don’t even have full-fledged family medicine departments. Students at these schools can study internal medicine, but many of those graduates end up choosing subspecialties like gastroenterology or cardiology.
One potential solution: eliminate tuition, in the hope that debt-free students will base their career choice on passion rather than paycheck. In 2024, two elite medical schools — the Albert Einstein College of Medicine and the Johns Hopkins University School of Medicine — announced that charitable donations are enabling them to waive tuition, joining a handful of other tuition-free schools.
But the contrast between the school Lo Cascio attends and the institution that founded it starkly illustrates the limitations of this approach. Neither charges tuition.
In 2024, two-thirds of students graduating from her Long Island school chose residencies in primary care. Lo Cascio said the tuition waiver wasn’t a deciding factor in choosing pediatrics, among the lowest-paid specialties, with an average annual income of $260,000, according to Medscape.
At the sister school, the Manhattan-based NYU Grossman School of Medicine, the majority of its 2024 graduates chose specialties like orthopedics (averaging $558,000 a year) or dermatology ($479,000).
Primary care typically gets little respect. Professors and peers alike admonish students: If you’re so smart, why would you choose primary care? Anand Chukka, 27, said he has heard that refrain regularly throughout his years as a student at Harvard Medical School. Even his parents, both PhD scientists, wondered if he was wasting his education by pursuing primary care.
Seemingly minor issues can influence students’ decisions, Chukka said. He recalls envying the students on hospital rotations who routinely were served lunch, while those in primary care settings had to fetch their own.
Despite such headwinds, Chukka, now in his final year, remains enthusiastic about primary care. He has long wanted to care for poor and other underserved people, and a one-year clerkship at a community practice serving low-income patients reinforced that plan.
When students look to the future, especially if they haven’t had such exposure, primary care can seem grim, burdened with time-consuming administrative tasks, such as seeking prior authorizations from insurers and grappling with electronic medical records.
While specialists may also face bureaucracy, primary care practices have it much worse: They have more patients and less money to hire help amid burgeoning paperwork requirements, said Caroline Richardson, chair of family medicine at Brown University’s Warren Alpert Medical School.
“It’s not the medical schools that are the problem; it’s the job,” Richardson said. “The job is too toxic.”
Kevin Grumbach, a professor of family and community medicine at the University of California-San Francisco, spent decades trying to boost the share of students choosing primary care, only to conclude: “There’s really very little that we can do in medical school to change people’s career trajectories.”
Instead, he said, the U.S. health care system must address the low pay and lack of support.
And yet, some schools find a way to produce significant proportions of primary care doctors — through recruitment and programs that provide positive experiences and mentors.
U.S. News & World Report recently ranked 168 medical schools by the percentage of graduates who were practicing primary care six to eight years after graduation.
The top 10 schools are all osteopathic medical schools, with 41% to 47% of their students still practicing primary care. Unlike allopathic medical schools, which award MD degrees, osteopathic schools, which award DO degrees, have a history of focusing on primary care and are graduating a growing share of the nation’s primary care physicians.
At the bottom of the U.S. News list is Yale, with 10.7% of its graduates finding lasting careers in primary care. Other elite schools have similar rates: Johns Hopkins, 13.1%; Harvard, 13.7%.
In contrast, public universities that have made it a mission to promote primary care have much higher numbers.
The University of Washington — No. 18 in the ranking, with 36.9% of graduates working in primary care — has a decades-old program placing students in remote parts of Washington, Wyoming, Alaska, Montana, and Idaho. UW recruits students from those areas, and many go back to practice there, with more than 20% of graduates settling in rural communities, according to Joshua Jauregui, assistant dean for clinical curriculum.
Likewise, the University of California-Davis (No. 22, with 36.3% of graduates in primary care) increased the percentage of students choosing family medicine from 12% in 2009 to 18% in 2023, even as it ranks high in specialty training. Programs such as an accelerated three-year primary care “pathway,” which enrolls primarily first-generation college students, help sustain interest in non-specialty medical fields.
The effort starts with recruitment, looking beyond test scores to the life experiences that forge the compassionate, humanistic doctors most needed in primary care, said Mark Henderson, associate dean for admissions and outreach. Most of the students have families who struggle to get primary care, he said. “So they care a lot about it, and it’s not just an intellectual, abstract sense.”
Establishing schools dedicated to primary care, like the one on Long Island, is not a solution in the eyes of some advocates, who consider primary care the backbone of medicine and not a separate discipline. Toyese Oyeyemi Jr., executive director of the Social Mission Alliance at the Fitzhugh Mullan Institute of Health Workforce Equity, worries that establishing such schools might let others “off the hook.”
Still, attending a medical school created to produce primary care doctors worked out well for Lo Cascio. Although she underwent the usual specialty rotations, her passion for pediatrics never flagged — owing to her 23 classmates, two mentors, and her first-year clerkship shadowing a community pediatrician. Now, she’s applying for pediatric residencies.
Lo Cascio also has deep personal reasons: Throughout her experience with a congenital heart condition, her pediatrician was a “guiding light.”
“No matter what else has happened in school, in life, in the world, and medically, your pediatrician is the person that you can come back to,” she said. “What a beautiful opportunity it would be to be that for someone else.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Gut Renovation – by Dr. Roshini Raj, with Sheila Buff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless we actually feel something going on down there, gut health is an oft-neglected part of overall health—which is unfortunate, because invisible as it may often be, it affects so much.
Gastroenterologist Dr. Roshini Raj gives us all the need-to-know information, explanations of why things happen the way they do with regard to the gut, and tips, tricks, and hacks to improve matters.
She also does some mythbusting along the way, and advises about what things don’t make a huge difference, including what medications don’t have a lot of evidence for their usefulness.
The style is easy-reading pop-science, with plenty of high-quality medical content.
Reading between the lines, a lot of the book as it stands was probably written by the co-author, Sheila Buff, who is a professional ghostwriter and specializes in working closely with doctors to produce works that are readable and informative to the layperson while still being full of the doctor’s knowledge and expertise. So a reasonable scenario is that Dr. Raj gave her extensive notes, she took it from there, passed it back to her for medical corrections, and they had a little back and forth until it was done. Whatever their setup, the end result was definitely good!
Bottom line: if you’d like a guide to gut health that’s practical and easy to read, while being quite comprehensive and certainly a lot more than “eat probiotics and fiber”, then this book is a fine choice.
Share This Post
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Chorus or Cacophony? Cicada Song Hits Some Ears Harder Than Others
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Shhhooo. Wee-uuu. Chick, chick, chick. That’s the sound of three different cicada species. For some people, those sounds are the song of the summer. Others wish the insects would turn it down. The cacophony can be especially irritating for people on the autism spectrum who have hearing sensitivity.
Warren Rickly, 14, lives in suburban south St. Louis County, Missouri. Warren, who has autism, was at the bus stop recently waiting for his younger brother when the sound of cicadas became too much to bear.
“He said it sounds like there’s always a train running next to him,” his mother, Jamie Reed, said.
Warren told her the noise hurt.
Starting this spring, trillions of the red-eyed insects crawled their way out of the ground across the Midwest and Southeast. It’s part of a rare simultaneous emergence of two broods — one that appears every 13 years, the other every 17.
The noisy insects can be stressful. People with autism can have a sensitivity to texture, brightness, and sound.
“I think the difference for individuals with autism is the level of intensity or how upsetting some of these sensory differences are,” said Rachel Follmer, a developmental and behavioral pediatrician at Lurie Children’s Hospital in Chicago.
“It can get to the extreme where it can cause physical discomfort,” she said.
When a large group of cicadas starts to sing, the chorus can be as loud as a motorcycle. Researchers at the University of Missouri-St. Louis this year crowdsourced cicada noise levels as high as 86 decibels, about as loud as a food blender.
That can be stressful, not melodic, Follmer said.
To help children cope, she suggests giving them a primer before they encounter a noisy situation. For cicadas, that could mean explaining what they are, that they don’t bite or sting, and that they’ll be here for just a short time.
“When something is uncomfortable, not having power in that situation can be very scary for a lot of individuals, whether you’re on the spectrum or not,” Follmer said.
Jamie Reed’s family has been using this and other strategies to help her son. Warren wears noise-canceling headphones, listens to music, and has been teaching himself about cicadas.
“For him, researching it and looking into it I think grounds him a little bit,” Reed said.
Fatima Husain is a professor and neuroscientist at the University of Illinois Urbana-Champaign and studies how the brain processes sound. She said people with tinnitus may also struggle with cicada song.
Tinnitus, a ringing or other noise in the ears, is a person’s perception of sound without an external source.
“Some people say it sounds like buzzing, like wind blowing through trees, and ironically, quite a few people say it sounds like cicadas,” Husain said.
For most people with tinnitus the cicada’s song is harmless background noise, according to Husain, but for others the ringing can prevent easy conversation or sleep. Those with tinnitus are also more likely to have anxiety or depression. A loud persistent sound, like singing cicadas, can make someone’s tinnitus worse, Husain said.
It’s not always bad, though. The cicada’s song can also be a relief.
For some, tinnitus gets worse in a quiet environment. Husain said she’s seen reports this year of patients saying the cicadas’ song has been like soothing white noise.
“The sound is loud enough that in some ways it’s drowning their internal tinnitus,” Husain said.
As loud as the cicadas can be, they won’t necessarily damage anyone’s hearing, according to the Centers for Disease Control and Prevention. Hearing loss builds up over time from repeated exposure to loud sounds. Cicadas aren’t loud enough for long enough to do lasting damage, Husain said.
Everyday sources of noise come with a higher risk. Husain said constant exposure to loud highways, an airport, industrial sites, or household appliances like blenders and hair dryers can be a concern. And they can take a toll on someone’s emotional well-being.
“If you are being exposed to very loud sounds for a part of your school day or your working day, it may make you more stressed out; it may make you more angry about things,” she said.
Unlike the highway or an airport, cicadas won’t be around long. Most of the current brood will be gone in the next few weeks. Just in time for another noisy summer event: the Fourth of July.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Say That Again: Using Hearing Aids Can Be Frustrating for Older Adults, but Necessary
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It was an every-other-day routine, full of frustration.
Every time my husband called his father, who was 94 when he died in 2022, he’d wait for his dad to find his hearing aids and put them in before they started talking.
Even then, my father-in-law could barely hear what my husband was saying. “What?” he’d ask over and over.
Then, there were the problems my father-in-law had replacing the devices’ batteries. And the times he’d end up in the hospital, unable to understand what people were saying because his hearing aids didn’t seem to be functioning. And the times he’d drop one of the devices and be unable to find it.
How many older adults have problems of this kind?
There’s no good data about this topic, according to Nicholas Reed, an assistant professor of epidemiology at Johns Hopkins Bloomberg School of Public Health who studies hearing loss. He did a literature search when I posed the question and came up empty.
Reed co-authored the most definitive study to date of hearing issues in older Americans, published in JAMA Open Network last year. Previous studies excluded people 80 and older. But data became available when a 2021 survey by the National Health and Aging Trends Study included hearing assessments conducted at people’s homes.
The results, based on a nationally representative sample of 2,803 people 71 and older, are eye-opening. Hearing problems become pervasive with advancing age, exceeding 90% in people 85 and older, compared with 53% of 71- to 74-year-olds. Also, hearing worsens over time, with more people experiencing moderate or severe deficits once they reach or exceed age 80, compared with people in their 70s.
However, only 29% of those with hearing loss used hearing aids. Multiple studies have documented barriers that inhibit use. Such devices, which Medicare doesn’t cover, are pricey, from nearly $1,000 for a good over-the-counter set (OTC hearing aids became available in 2022) to more than $6,000 for some prescription models. In some communities, hearing evaluation services are difficult to find. Also, people often associate hearing aids with being old and feel self-conscious about wearing them. And they tend to underestimate hearing problems that develop gradually.
Barbara Weinstein, a professor of audiology at the City University of New York Graduate Center and author of the textbook “Geriatric Audiology,” added another concern to this list when I reached out to her: usability.
“Hearing aids aren’t really designed for the population that most needs to use them,” she told me. “The move to make devices smaller and more sophisticated technologically isn’t right for many people who are older.”
That’s problematic because hearing loss raises the risk of cognitive decline, dementia, falls, depression, and social isolation.
What advice do specialists in hearing health have for older adults who have a hard time using their hearing aids? Here are some thoughts they shared.
Consider larger, customized devices. Many older people, especially those with arthritis, poor fine motor skills, compromised vision, and some degree of cognitive impairment, have a hard time manipulating small hearing aids and using them properly.
Lindsay Creed, associate director of audiology practices at the American Speech-Language-Hearing Association, said about half of her older clients have “some sort of dexterity issue, whether numbness or reduced movement or tremor or a lack of coordination.” Shekinah Mast, owner of Mast Audiology Services in Seaford, Delaware, estimates nearly half of her clients have vision issues.
For clients with dexterity challenges, Creed often recommends “behind-the-ear hearing aids,” with a loop over the ear, and customized molds that fit snugly in the ear. Customized earpieces are larger than standardized models.
“The more dexterity challenges you have, the better you’ll do with a larger device and with lots of practice picking it up, orienting it, and putting it in your ear,” said Marquitta Merkison, associate director of audiology practices at ASHA.
For older people with vision issues, Mast sometimes orders hearing aids in different colors for different ears. Also, she’ll help clients set up stands at home for storing devices, chargers, and accessories so they can readily find them each time they need them.
Opt for ease of use. Instead of buying devices that require replacing tiny batteries, select a device that can be charged overnight and operate for at least a day before being recharged, recommended Thomas Powers, a consultant to the Hearing Industries Association. These are now widely available.
People who are comfortable using a smartphone should consider using a phone app to change volume and other device settings. Dave Fabry, chief hearing health officer at Starkey, a major hearing aid manufacturer, said he has patients in their 80s and 90s “who’ve found that being able to hold a phone and use larger visible controls is easier than manipulating the hearing aid.”
If that’s too difficult, try a remote control. GN ReSound, another major manufacturer, has designed one with two large buttons that activate the volume control and programming for its hearing aids, said Megan Quilter, the company’s lead audiologist for research and development.
Check out accessories. Say you’re having trouble hearing other people in restaurants. You can ask the person across the table to clip a microphone to his shirt or put the mike in the center of the table. (The hearing aids will need to be programmed to allow the sound to be streamed to your ears.)
Another low-tech option: a hearing aid clip that connects to a piece of clothing to prevent a device from falling to the floor if it becomes dislodged from the ear.
Wear your hearing aids all day. “The No. 1 thing I hear from older adults is they think they don’t need to put on their hearing aids when they’re at home in a quiet environment,” said Erika Shakespeare, who owns Audiology and Hearing Aid Associates in La Grande, Oregon.
That’s based on a misunderstanding. Our brains need regular, not occasional, stimulation from our environments to optimize hearing, Shakespeare explained. This includes noises in seemingly quiet environments, such as the whoosh of a fan, the creak of a floor, or the wind’s wail outside a window.
“If the only time you wear hearing aids is when you think you need them, your brain doesn’t know how to process all those sounds,” she told me. Her rule of thumb: “Wear hearing aids all your waking hours.”
Consult a hearing professional. Everyone’s needs are different, so it’s a good idea to seek out an audiologist or hearing specialist who, for a fee, can provide guidance.
“Most older people are not going to know what they need” and what options exist without professional assistance, said Virginia Ramachandran, the head of audiology at Oticon, a major hearing aid manufacturer, and a past president of the American Academy of Audiology.
Her advice to older adults: Be “really open” about your challenges.
If you can’t afford hearing aids, ask a hearing professional for an appointment to go over features you should look for in over-the-counter devices. Make it clear you want the appointment to be about your needs, not a sales pitch, Reed said. Audiology practices don’t routinely offer this kind of service, but there’s good reason to ask since Medicare started covering once-a-year audiologist consultations last year.
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
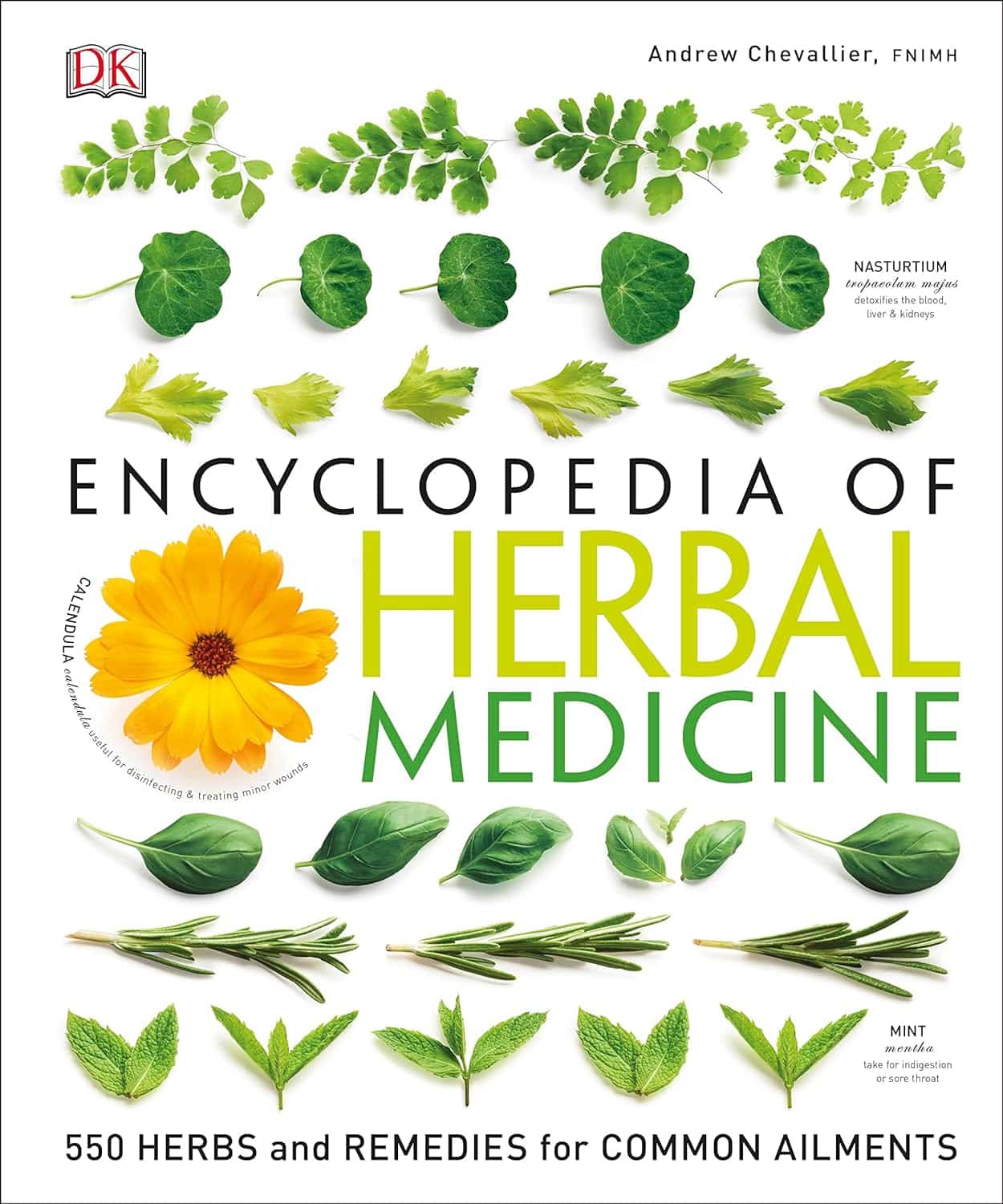
Encyclopedia Of Herbal Medicine – by Andrew Chevallier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A common problem with a lot of herbal medicine is it’s “based on traditional use only”, while on the other hand, learning about the actual science of it can mean poring through stacks of Randomized Clinical Trials, half of which are paywalled.
This beautifully and clearly-illustrated book bridges that gap. It gives not just the history, but also the science, of the use of many medicinal herbs (spotlight on 100 key ones; details on 450 more).
It gives advice on growing, harvesting, processing, and using the herbs, as well as what not to do (with regard to safety). And in case you don’t fancy yourself a gardener, you’ll also find advice on places one can buy herbs, and what you’ll need to know to choose them well (controlling for quality etc).
You can read it cover-to-cover, or look up what you need by plant in its general index, or by ailment (200 common ailments listed). As for its bibliography, it does list many textbooks, but not individual papers—though it does cite 12 popular scientific journals too.
Bottom line: if you want a good, science-based, one-stop book for herbal medicine, this is a top-tier choice.
Click here to check out the Encyclopedia of Herbal Medicine, and expand your home remedy repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: