7 Days Of Celery Juice: What’s The Verdict?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Laura “Try” tries many popular trends, and reports on the benefits (or problems, or both). In this case, it’s 7 days of celery juice… Not as a fast, though, i.e. she doesn’t just have celery juice for 7 days, but rather, it’s how she kicks off each morning, with half a liter (16oz) on an empty stomach.
What she found
First, she bought a masticating juicer and organic celery. So, those are expenses to consider, especially the one-off expense of the juicer, and the ongoing expense of organic celery—estimated $90/month).
In terms of taste, she was surprised it wasn’t as bitter as expected, but from the second day onwards, she did use the juicer’s filter to remove the frothy sludge, and she also switched to juicing only the stalks, not the leaves—which are more bitter.
10almonds note: the leaves are more bitter because that’s where the polyphenols are more densely concentrated. The leaves are better for you than the stalks. Enjoy the leaves. Really: if you chop them finely you can use them as herbs in your cooking, and if you’re making a salad, just chop them into that too.
The reason she picked the quantity of half a liter is because this is what she found recommended to coat the stomach lining—on the promise of increased stomach acid production, reduced bacteria overgrowth, as well as antiviral, antifungal, and anti-inflammatory properties. As she’s just one woman without a personal lab, she couldn’t test and thus verify any of these though—but she did still have benefits to report:
She did experience clearer skin, more energy, and better sleep after a few days.
Ultimately, she decided to continue to do it just at the weekends, due to its positive effects, despite the cost and time consumption.
For more personal insights, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Enjoy Bitter Foods For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Think you’re good at multi-tasking? Here’s how your brain compensates – and how this changes with age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re all time-poor, so multi-tasking is seen as a necessity of modern living. We answer work emails while watching TV, make shopping lists in meetings and listen to podcasts when doing the dishes. We attempt to split our attention countless times a day when juggling both mundane and important tasks.
But doing two things at the same time isn’t always as productive or safe as focusing on one thing at a time.
The dilemma with multi-tasking is that when tasks become complex or energy-demanding, like driving a car while talking on the phone, our performance often drops on one or both.
Here’s why – and how our ability to multi-task changes as we age.
Doing more things, but less effectively
The issue with multi-tasking at a brain level, is that two tasks performed at the same time often compete for common neural pathways – like two intersecting streams of traffic on a road.
In particular, the brain’s planning centres in the frontal cortex (and connections to parieto-cerebellar system, among others) are needed for both motor and cognitive tasks. The more tasks rely on the same sensory system, like vision, the greater the interference.
This is why multi-tasking, such as talking on the phone, while driving can be risky. It takes longer to react to critical events, such as a car braking suddenly, and you have a higher risk of missing critical signals, such as a red light.
The more involved the phone conversation, the higher the accident risk, even when talking “hands-free”.
Generally, the more skilled you are on a primary motor task, the better able you are to juggle another task at the same time. Skilled surgeons, for example, can multitask more effectively than residents, which is reassuring in a busy operating suite.
Highly automated skills and efficient brain processes mean greater flexibility when multi-tasking.
Adults are better at multi-tasking than kids
Both brain capacity and experience endow adults with a greater capacity for multi-tasking compared with children.
You may have noticed that when you start thinking about a problem, you walk more slowly, and sometimes to a standstill if deep in thought. The ability to walk and think at the same time gets better over childhood and adolescence, as do other types of multi-tasking.
When children do these two things at once, their walking speed and smoothness both wane, particularly when also doing a memory task (like recalling a sequence of numbers), verbal fluency task (like naming animals) or a fine-motor task (like buttoning up a shirt). Alternately, outside the lab, the cognitive task might fall by wayside as the motor goal takes precedence.
Brain maturation has a lot to do with these age differences. A larger prefrontal cortex helps share cognitive resources between tasks, thereby reducing the costs. This means better capacity to maintain performance at or near single-task levels.
The white matter tract that connects our two hemispheres (the corpus callosum) also takes a long time to fully mature, placing limits on how well children can walk around and do manual tasks (like texting on a phone) together.
For a child or adult with motor skill difficulties, or developmental coordination disorder, multi-tastking errors are more common. Simply standing still while solving a visual task (like judging which of two lines is longer) is hard. When walking, it takes much longer to complete a path if it also involves cognitive effort along the way. So you can imagine how difficult walking to school could be.
What about as we approach older age?
Older adults are more prone to multi-tasking errors. When walking, for example, adding another task generally means older adults walk much slower and with less fluid movement than younger adults.
These age differences are even more pronounced when obstacles must be avoided or the path is winding or uneven.
Older adults tend to enlist more of their prefrontal cortex when walking and, especially, when multi-tasking. This creates more interference when the same brain networks are also enlisted to perform a cognitive task.
These age differences in performance of multi-tasking might be more “compensatory” than anything else, allowing older adults more time and safety when negotiating events around them.
Older people can practise and improve
Testing multi-tasking capabilities can tell clinicians about an older patient’s risk of future falls better than an assessment of walking alone, even for healthy people living in the community.
Testing can be as simple as asking someone to walk a path while either mentally subtracting by sevens, carrying a cup and saucer, or balancing a ball on a tray.
Patients can then practise and improve these abilities by, for example, pedalling an exercise bike or walking on a treadmill while composing a poem, making a shopping list, or playing a word game.
The goal is for patients to be able to divide their attention more efficiently across two tasks and to ignore distractions, improving speed and balance.
There are times when we do think better when moving
Let’s not forget that a good walk can help unclutter our mind and promote creative thought. And, some research shows walking can improve our ability to search and respond to visual events in the environment.
But often, it’s better to focus on one thing at a time
We often overlook the emotional and energy costs of multi-tasking when time-pressured. In many areas of life – home, work and school – we think it will save us time and energy. But the reality can be different.
Multi-tasking can sometimes sap our reserves and create stress, raising our cortisol levels, especially when we’re time-pressured. If such performance is sustained over long periods, it can leave you feeling fatigued or just plain empty.
Deep thinking is energy demanding by itself and so caution is sometimes warranted when acting at the same time – such as being immersed in deep thought while crossing a busy road, descending steep stairs, using power tools, or climbing a ladder.
So, pick a good time to ask someone a vexed question – perhaps not while they’re cutting vegetables with a sharp knife. Sometimes, it’s better to focus on one thing at a time.
Peter Wilson, Professor of Developmental Psychology, Australian Catholic University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
A new emergency procedure for cardiac arrests aims to save more lives – here’s how it works
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As of January this year, Aotearoa New Zealand became just the second country (after Canada) to adopt a groundbreaking new procedure for patients experiencing cardiac arrest.
Known as “double sequential external defibrillation” (DSED), it will change initial emergency response strategies and potentially improve survival rates for some patients.
Surviving cardiac arrest hinges crucially on effective resuscitation. When the heart is working normally, electrical pulses travel through its muscular walls creating regular, co-ordinated contractions.
But if normal electrical rhythms are disrupted, heartbeats can become unco-ordinated and ineffective, or cease entirely, leading to cardiac arrest.
Defibrillation is a cornerstone resuscitation method. It gives the heart a powerful electric shock to terminate the abnormal electrical activity. This allows the heart to re-establish its regular rhythm.
Its success hinges on the underlying dysfunctional heart rhythm and the proper positioning of the defibrillation pads that deliver the shock. The new procedure will provide a second option when standard positioning is not effective.
Using two defibrillators
During standard defibrillation, one pad is placed on the right side of the chest just below the collarbone. A second pad is placed below the left armpit. Shocks are given every two minutes.
Early defibrillation can dramatically improve the likelihood of surviving a cardiac arrest. However, around 20% of patients whose cardiac arrest is caused by “ventricular fibrillation” or “pulseless ventricular tachycardia” do not respond to the standard defibrillation approach. Both conditions are characterised by abnormal activity in the heart ventricles.
DSED is a novel method that provides rapid sequential shocks to the heart using two defibrillators. The pads are attached in two different locations: one on the front and side of the chest, the other on the front and back.
A single operator activates the defibrillators in sequence, with one hand moving from the first to the second. According to a recent randomised trial in Canada, this approach could more than double the chances of survival for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard shocks.
The second shock is thought to improve the chances of eliminating persistent abnormal electrical activity. It delivers more total energy to the heart, travelling along a different pathway closer to the heart’s left ventricle.
Evidence of success
New Zealand ambulance data from 2020 to 2023 identified about 1,390 people who could potentially benefit from novel defibrillation methods. This group has a current survival rate of only 14%.
Recognising the potential for DSED to dramatically improve survival for these patients, the National Ambulance Sector Clinical Working Group updated the clinical procedures and guidelines for emergency medical services personnel.
The guidelines now specify that if ventricular fibrillation or pulseless ventricular tachycardia persist after two shocks with standard defibrillation, the DSED method should be administered. Two defibrillators need to be available, and staff must be trained in the new approach.
Though the existing evidence for DSED is compelling, until recently it was based on theory and a small number of potentially biased observational studies. The Canadian trial was the first to directly compare DSED to standard treatment.
From a total of 261 patients, 30.4% treated with this strategy survived, compared to 13.3% when standard resuscitation protocols were followed.
The design of the trial minimised the risk of other factors confounding results. It provides confidence that survival improvements were due to the defibrillation approach and not regional differences in resources and training.
The study also corroborates and builds on existing theoretical and clinical scientific evidence. As the trial was stopped early due to the COVID-19 pandemic, however, the researchers could recruit fewer than half of the numbers planned for the study.
Despite these and other limitations, the international group of experts that advises on best practice for resuscitation updated its recommendations in 2023 in response to the trial results. It suggested (with caution) that emergency medical services consider DSED for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard treatment.
Training and implementation
Although the evidence is still emerging, implementation of DSED by emergency services in New Zealand has implications beyond the care of patients nationally. It is also a key step in advancing knowledge about optimal resuscitation strategies globally.
There are always concerns when translating an intervention from a controlled research environment to the relative disorder of the real world. But the balance of evidence was carefully considered before making the decision to change procedures for a group of patients who have a low likelihood of survival with current treatment.
Before using DSED, emergency medical personnel undergo mandatory education, simulation and training. Implementation is closely monitored to determine its impact.
Hospitals and emergency departments have been informed of the protocol changes and been given opportunities to ask questions and give feedback. As part of the implementation, the St John ambulance service will perform case reviews in addition to wider monitoring to ensure patient safety is prioritised.
Ultimately, those involved are optimistic this change to cardiac arrest management in New Zealand will have a positive impact on survival for affected patients.
Vinuli Withanarachchie, PhD candidate, College of Health, Massey University; Bridget Dicker, Associate Professor of Paramedicine, Auckland University of Technology, and Sarah Maessen, Research Associate, Auckland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What’s the difference between a food allergy and an intolerance?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At one time or another, you’ve probably come across someone who is lactose intolerant and might experience some unpleasant gut symptoms if they have dairy. Maybe it’s you – food intolerances are estimated to affect up to 25% of Australians.
Meanwhile, cow’s milk allergy is one of the most common food allergies in infants and young children, affecting around one in 100 infants.
But what’s the difference between food allergies and food intolerances? While they might seem alike, there are some fundamental differences between the two.
Feel good studio/Shutterstock What is an allergy?
Australia has one of the highest rates of food allergies in the world. Food allergies can develop at any age but are more common in children, affecting more than 10% of one-year-olds and 6% of children at age ten.
A food allergy happens when the body’s immune system mistakenly reacts to certain foods as if they were dangerous. The most common foods that trigger allergies include eggs, peanuts and other nuts, milk, shellfish, fish, soy and wheat.
Mild to moderate signs of food allergy include a swollen face, lips or eyes; hives or welts on your skin; or vomiting. A severe allergic reaction (called anaphylaxis) can cause trouble breathing, persistent dizziness or collapse.
What is an intolerance?
Food intolerances (sometimes called non-allergic reactions) are also reactions to food, but they don’t involve your immune system.
For example, lactose intolerance is a metabolic condition that happens when the body doesn’t produce enough lactase. This enzyme is needed to break down the lactose (a type of sugar) in dairy products.
Food intolerances can also include reactions to natural chemicals in foods (such as salicylates, found in some fruits, vegetables, herbs and spices) and problems with artificial preservatives or flavour enhancers.
Lactose intolerance is caused by a problem with breaking down lactose in milk. Pormezz/Shutterstock Symptoms of food intolerances can include an upset stomach, headaches and fatigue, among others.
Food intolerances don’t cause life-threatening reactions (anaphylaxis) so are less dangerous than allergies in the short term, although they can cause problems in the longer term such as malnutrition.
We don’t know a lot about how common food intolerances are, but they appear to be more commonly reported than allergies. They can develop at any age.
It can be confusing
Some foods, such as peanuts and tree nuts, are more often associated with allergy. Other foods or ingredients, such as caffeine, are more often associated with intolerance.
Meanwhile, certain foods, such as cow’s milk and wheat or gluten (a protein found in wheat, rye and barley), can cause both allergic and non-allergic reactions in different people. But these reactions, even when they’re caused by the same foods, are quite different.
For example, children with a cow’s milk allergy can react to very small amounts of milk, and serious reactions (such as throat swelling or difficulty breathing) can happen within minutes. Conversely, many people with lactose intolerance can tolerate small amounts of lactose without symptoms.
There are other differences too. Cow’s milk allergy is more common in children, though many infants will grow out of this allergy during childhood.
Lactose intolerance is more common in adults, but can also sometimes be temporary. One type of lactose intolerance, secondary lactase deficiency, can be caused by damage to the gut after infection or with medication use (such as antibiotics or cancer treatment). This can go away by itself when the underlying condition resolves or the person stops using the relevant medication.
Whether an allergy or intolerance is likely to be lifelong depends on the food and the reason that the child or adult is reacting to it.
Allergies to some foods, such as milk, egg, wheat and soy, often resolve during childhood, whereas allergies to nuts, fish or shellfish, often (but not always) persist into adulthood. We don’t know much about how likely children are to grow out of different types of food intolerances.
How do you find out what’s wrong?
If you think you may have a food allergy or intolerance, see a doctor.
Allergy tests help doctors find out which foods might be causing your allergic reactions (but can’t diagnose food intolerances). There are two common types: skin prick tests and blood tests.
In a skin prick test, doctors put tiny amounts of allergens (the things that can cause allergies) on your skin and make small pricks to see if your body reacts.
A blood test checks for allergen-specific immunoglobulin E (IgE) antibodies in your blood that show if you might be allergic to a particular food.
Blood tests can help diagnose allergies. RossHelen/Shutterstock Food intolerances can be tricky to figure out because the symptoms depend on what foods you eat and how much. To diagnose them, doctors look at your health history, and may do some tests (such as a breath test). They may ask you to keep a record of foods you eat and timing of symptoms.
A temporary elimination diet, where you stop eating certain foods, can also help to work out which foods you might be intolerant to. But this should only be done with the help of a doctor or dietitian, because eliminating particular foods can lead to nutritional deficiencies, especially in children.
Is there a cure?
There’s currently no cure for food allergies or intolerances. For allergies in particular, it’s important to strictly avoid allergens. This means reading food labels carefully and being vigilant when eating out.
However, researchers are studying a treatment called oral immunotherapy, which may help some people with food allergies become less sensitive to certain foods.
Whether you have a food allergy or intolerance, your doctor or dietitian can help you to make sure you’re eating the right foods.
Victoria Gibson, a Higher Degree by Research student and Research Officer at the School of Nursing, Midwifery and Social Work at the University of Queensland, and Rani Scott-Farmer, a Senior Research Assistant at the University of Queensland, contributed to this article.
Jennifer Koplin, Group Leader, Childhood Allergy & Epidemiology, The University of Queensland and Desalegn Markos Shifti, Postdoctoral Research Fellow, Child Health Research Centre, Faculty of Medicine, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
If I’m diagnosed with one cancer, am I likely to get another?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Receiving a cancer diagnosis is life-changing and can cause a range of concerns about ongoing health.
Fear of cancer returning is one of the top health concerns. And managing this fear is an important part of cancer treatment.
But how likely is it to get cancer for a second time?
Why can cancer return?
While initial cancer treatment may seem successful, sometimes a few cancer cells remain dormant. Over time, these cancer cells can grow again and may start to cause symptoms.
This is known as cancer recurrence: when a cancer returns after a period of remission. This period could be days, months or even years. The new cancer is the same type as the original cancer, but can sometimes grow in a new location through a process called metastasis.
Actor Hugh Jackman has gone public about his multiple diagnoses of basal cell carcinoma (a type of skin cancer) over the past decade.
The exact reason why cancer returns differs depending on the cancer type and the treatment received. Research is ongoing to identify genes associated with cancers returning. This may eventually allow doctors to tailor treatments for high-risk people.
What are the chances of cancer returning?
The risk of cancer returning differs between cancers, and between sub-types of the same cancer.
New screening and treatment options have seen reductions in recurrence rates for many types of cancer. For example, between 2004 and 2019, the risk of colon cancer recurring dropped by 31-68%. It is important to remember that only someone’s treatment team can assess an individual’s personal risk of cancer returning.
For most types of cancer, the highest risk of cancer returning is within the first three years after entering remission. This is because any leftover cancer cells not killed by treatment are likely to start growing again sooner rather than later. Three years after entering remission, recurrence rates for most cancers decrease, meaning that every day that passes lowers the risk of the cancer returning.
Every day that passes also increases the numbers of new discoveries, and cancer drugs being developed.
What about second, unrelated cancers?
Earlier this year, we learned Sarah Ferguson, Duchess of York, had been diagnosed with malignant melanoma (a type of skin cancer) shortly after being treated for breast cancer.
Although details have not been confirmed, this is likely a new cancer that isn’t a recurrence or metastasis of the first one.
Australian research from Queensland and Tasmania shows adults who have had cancer have around a 6-36% higher risk of developing a second primary cancer compared to the risk of cancer in the general population.
Who’s at risk of another, unrelated cancer?
With improvements in cancer diagnosis and treatment, people diagnosed with cancer are living longer than ever. This means they need to consider their long-term health, including their risk of developing another unrelated cancer.
Reasons for such cancers include different types of cancers sharing the same kind of lifestyle, environmental and genetic risk factors.
The increased risk is also likely partly due to the effects that some cancer treatments and imaging procedures have on the body. However, this increased risk is relatively small when compared with the (sometimes lifesaving) benefits of these treatment and procedures.
While a 6-36% greater chance of getting a second, unrelated cancer may seem large, only around 10-12% of participants developed a second cancer in the Australian studies we mentioned. Both had a median follow-up time of around five years.
Similarly, in a large US study only about one in 12 adult cancer patients developed a second type of cancer in the follow-up period (an average of seven years).
The kind of first cancer you had also affects your risk of a second, unrelated cancer, as well as the type of second cancer you are at risk of. For example, in the two Australian studies we mentioned, the risk of a second cancer was greater for people with an initial diagnosis of head and neck cancer, or a haematological (blood) cancer.
People diagnosed with cancer as a child, adolescent or young adult also have a greater risk of a second, unrelated cancer.
What can I do to lower my risk?
Regular follow-up examinations can give peace of mind, and ensure any subsequent cancer is caught early, when there’s the best chance of successful treatment.
Maintenance therapy may be used to reduce the risk of some types of cancer returning. However, despite ongoing research, there are no specific treatments against cancer recurrence or developing a second, unrelated cancer.
But there are things you can do to help lower your general risk of cancer – not smoking, being physically active, eating well, maintaining a healthy body weight, limiting alcohol intake and being sun safe. These all reduce the chance of cancer returning and getting a second cancer.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, Walter and Eliza Hall Institute and Terry Boyle, Senior Lecturer in Cancer Epidemiology, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Viruses aren’t always harmful. 6 ways they’re used in health care and pest control
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We tend to just think of viruses in terms of their damaging impacts on human health and lives. The 1918 flu pandemic killed around 50 million people. Smallpox claimed 30% of those who caught it, and survivors were often scarred and blinded. More recently, we’re all too familiar with the health and economic impacts of COVID.
But viruses can also be used to benefit human health, agriculture and the environment.
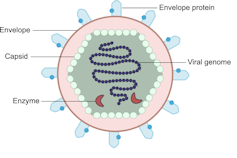
Viruses are comparatively simple in structure, consisting of a piece of genetic material (RNA or DNA) enclosed in a protein coat (the capsid). Some also have an outer envelope.
Viruses get into your cells and use your cell machinery to copy themselves.
Here are six ways we’ve harnessed this for health care and pest control.1. To correct genes
Viruses are used in some gene therapies to correct malfunctioning genes. Genes are DNA sequences that code for a particular protein required for cell function.
If we remove viral genetic material from the capsid (protein coat) we can use the space to transport a “cargo” into cells. These modified viruses are called “viral vectors”.
Viruses consist of a piece of RNA or DNA enclosed in a protein coat called the capsid.
DEXiViral vectors can deliver a functional gene into someone with a genetic disorder whose own gene is not working properly.
Some genetic diseases treated this way include haemophilia, sickle cell disease and beta thalassaemia.
2. Treat cancer
Viral vectors can be used to treat cancer.
Healthy people have p53, a tumour-suppressor gene. About half of cancers are associated with the loss of p53.
Replacing the damaged p53 gene using a viral vector stops the cancerous cell from replicating and tells it to suicide (apoptosis).
Viral vectors can also be used to deliver an inactive drug to a tumour, where it is then activated to kill the tumour cell.
This targeted therapy reduces the side effects otherwise seen with cytotoxic (cell-killing) drugs.
We can also use oncolytic (cancer cell-destroying) viruses to treat some types of cancer.
Tumour cells have often lost their antiviral defences. In the case of melanoma, a modified herpes simplex virus can kill rapidly dividing melanoma cells while largely leaving non-tumour cells alone.
3. Create immune responses
Viral vectors can create a protective immune response to a particular viral antigen.
One COVID vaccine uses a modified chimp adenovirus (adenoviruses cause the common cold in humans) to transport RNA coding for the SARS-CoV-2 spike protein into human cells.
The RNA is then used to make spike protein copies, which stimulate our immune cells to replicate and “remember” the spike protein.
Then, when you are exposed to SARS-CoV-2 for real, your immune system can churn out lots of antibodies and virus-killing cells very quickly to prevent or reduce the severity of infection.
4. Act as vaccines
Viruses can be modified to act directly as vaccines themselves in several ways.
We can weaken a virus (for an attenuated virus vaccine) so it doesn’t cause infection in a healthy host but can still replicate to stimulate the immune response. The chickenpox vaccine works like this.
The Salk vaccine for polio uses a whole virus that has been inactivated (so it can’t cause disease).
Others use a small part of the virus such as a capsid protein to stimulate an immune response (subunit vaccines).
An mRNA vaccine packages up viral RNA for a specific protein that will stimulate an immune response.
5. Kill bacteria
Viruses can – in limited situations in Australia – be used to treat antibiotic-resistant bacterial infections.
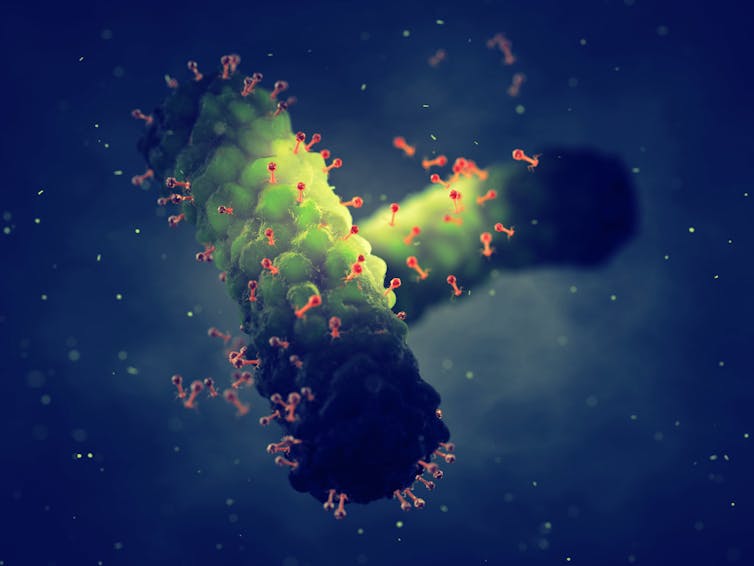
Bacteriophages are viruses that kill bacteria. Each type of phage usually infects a particular species of bacteria.
Unlike antibiotics – which often kill “good” bacteria along with the disease-causing ones – phage therapy leaves your normal flora (useful microbes) intact.
Bacteriophages (red) are viruses that kill bacteria (green).
Shutterstock6. Target plant, fungal or animal pests
Viruses can be species-specific (infecting one species only) and even cell-specific (infecting one type of cell only).
This occurs because the proteins viruses use to attach to cells have a shape that binds to a specific type of cell receptor or molecule, like a specific key fits a lock.
The virus can enter the cells of all species with this receptor/molecule. For example, rabies virus can infect all mammals because we share the right receptor, and mammals have other characteristics that allow infection to occur whereas other non-mammal species don’t.
When the receptor is only found on one cell type, then the virus will infect that cell type, which may only be found in one or a limited number of species. Hepatitis B virus successfully infects liver cells primarily in humans and chimps.
We can use that property of specificity to target invasive plant species (reducing the need for chemical herbicides) and pest insects (reducing the need for chemical insecticides). Baculoviruses, for example, are used to control caterpillars.
Similarly, bacteriophages can be used to control bacterial tomato and grapevine diseases.
Other viruses reduce plant damage from fungal pests.
Myxoma virus and calicivirus reduce rabbit populations and their environmental impacts and improve agricultural production.
Just like humans can be protected against by vaccination, plants can be “immunised” against a disease-causing virus by being exposed to a milder version.
Thea van de Mortel, Professor, Nursing, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
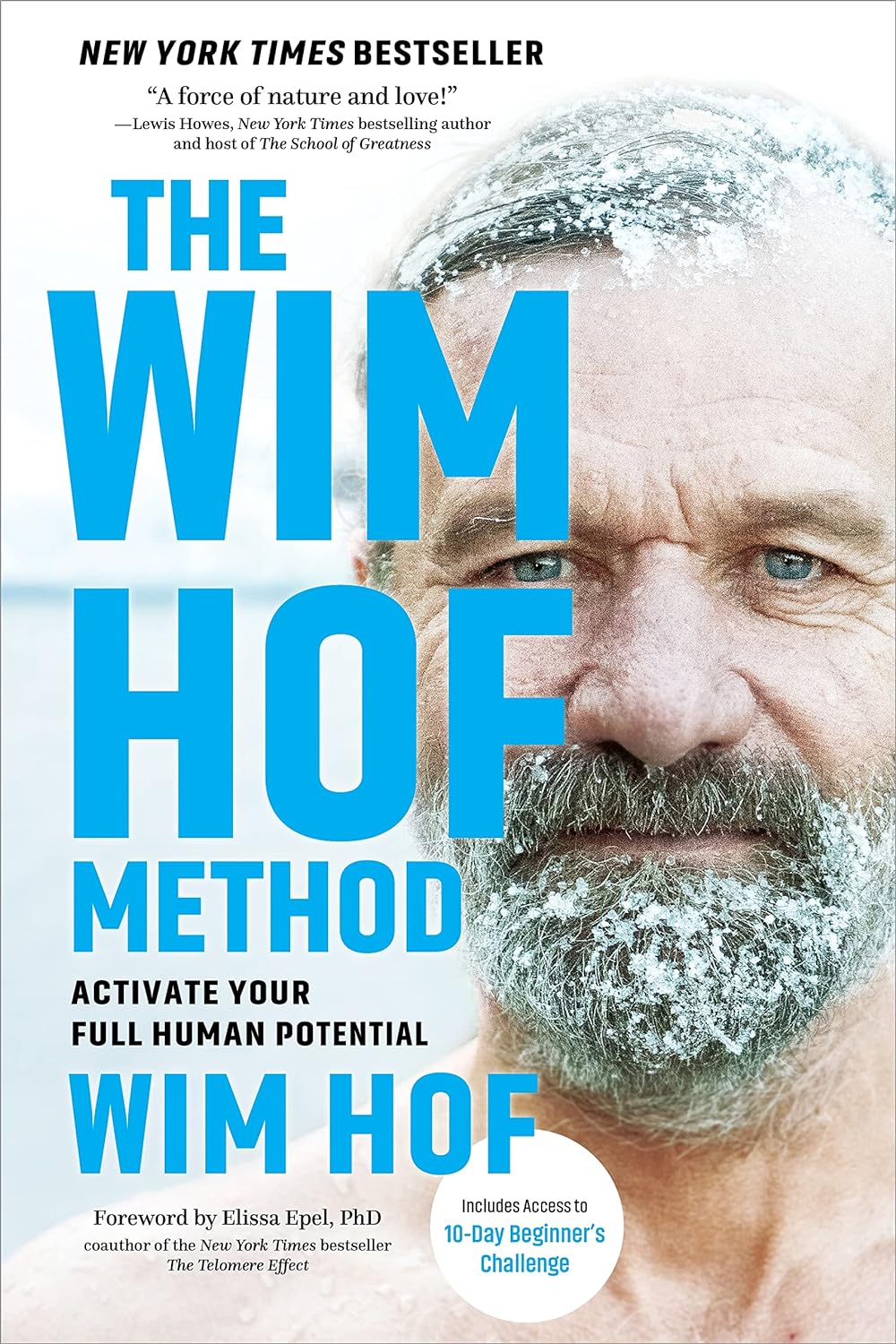
The Wim Hof Method – by Wim Hof
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Wednesday’s main feature, we wrote about the Wim Hof Method, and/but only scratched the surface. Such is the downside of being a super-condensed newsletter! However, it does give us the opportunity to feature the book:
The Wim Hof Method is definitely loudly trumpeted as “up there” with Atomic Habits or How Not To Die in the category of “life-changing” books. Why?
Firstly, it’s a very motivational book. Hof is a big proponent of the notion “if you think you can or you think you can’t, you’re right” idea, practises what he preaches, and makes clear he’s not special.
Secondly, it’s backed up with science. While it’s not a science-heavy book and that’s not the main focus, there are references to studies. Where physiological explanations are given for how certain things work, those explanations are sound. There’s no pseudoscience here, which is especially important for a book of this genre!
What does the book have that our article didn’t? A good few things:
- More about Hof’s own background and where it’s taken him. This is generally not a reason people buy books (unless they are biographies), but it’s interesting nonetheless.
- A lot more advice, data, and information about Cold Therapy and how it can (and, he argues convincingly, should) be built into your life.
- A lot about breathing exercises that we just didn’t cover at all in our article, but is actually an important part of the Wim Hof Method.
- More about stepping through the psychological barriers that can hold us back.
Bottom line: this book offers benefits that stretch into many areas of life, from some simple habits that can be built.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: