The Secret Easy Tips to Loosen Your Hips In 10 Minutes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff hips can often cause discomfort, and ultimately back pain because of how one thing relies on the other as its seat. However, there are ways to improve it without taking years to get to where you want to be:
One bit at a time
Warm up and massage:
- Massage the front and back of the thighs to loosen tight muscles.
- Use your body weight for effective massaging.
- Relax and breathe slowly while massaging.
Vary your stretches:
- Perform a seated butterfly stretch, but avoid overexertion.
- Move knees gently within a comfortable range of motion.
- Perform stretches like placing one foot on the opposite knee or holding legs to open hips.
- Stretch the hips while lying on the floor with bent knees.
And now for the “magic move”: lie on your stomach, bend one knee, and gently rock to loosen hip stiffness.
Generally speaking, for most stretches one can usually stretch further on one side at once, than both at the same time. So, leverage this in your flexibility training, to get each side of your body accustomed to going that bit further. Then, when your body is comfortable with that, put it together.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How Tight Are Your Hips? Test (And Fix!) With This
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spirulina vs Nori – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing spirulina to nori, we picked the nori.
Why?
In the battle of the seaweeds, if spirulina is a superfood (and it is), then nori is a super-dooperfood. So today is one of those “a very nutritious food making another very nutritious food look bad by standing next to it” days. With that in mind…
In terms of macros, they’re close to identical. They’re both mostly water with protein, carbs, and fiber. Technically nori is higher in carbs, but we’re talking about 2.5g/100g difference.
In the category of vitamins, spirulina has more vitamin B1, while nori has a lot more of vitamins A, B2, B3, B5, B6, B9, C, E, K, and choline.
When it comes to minerals, it’s a little closer but still a clear win for nori; spirulina has more copper, iron, and magnesium, while nori has more calcium, manganese, phosphorus, potassium, and zinc.
Want to try some nori? Here’s an example product on Amazon 😎
Want to learn more?
You might like to read:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori was an important part of the diet enjoyed here
Take care!
Share This Post
-
All In Your Head (Which Is Where It’s Supposed To Be)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s news is all about things above the neck, and mostly in the brain. From beating depression to beating cognitive decline, from mindfulness against pain to dentistry nightmares to avoid:
Transcranial ultrasound stimulation
Transcranial magnetic stimulation is one of those treatments that sounds like it’s out of a 1950s sci-fi novel, and yet, it actually works (it’s very well-evidenced against treatment-resistant depression, amongst other things). However, a weakness of it is that it’s difficult to target precisely, making modulation of most neurological disorders impossible. Using ultrasound instead of a magnetic field allows for much more finesse, with very promising initial results across a range of neurological disorders
Read in full: Transcranial ultrasound stimulation: a new frontier in non-invasive brain therapy
Related: Antidepressants: Personalization Is Key!
This may cause more pain and damage, but at least it’s more expensive too…
While socialized healthcare systems sometimes run into the problem of not wanting to spend money where it actually is needed, private healthcare systems have the opposite problem: there’s a profit incentive to upsell to more expensive treatments. Here’s how that’s played out in dentistry:
Read in full: Dentists are pulling healthy and treatable teeth to profit from implants, experts warn
Related: Tooth Remineralization: How To Heal Your Teeth Naturally
Mindfulness vs placebo, for pain
It can be difficult with some “alternative therapies” to test against placebo, for example “and control group B will merely believe that they are being pierced with needles”, etc. However, in this case, mindfulness meditation was tested as an analgesic vs sham meditation (just deep breathing) and also vs placebo analgesic cream, vs distraction (listening to an audiobook). Mindfulness meditation beat all of the other things:
Read in full: Mindfulness meditation outperforms placebo in reducing pain
Related: No-Frills, Evidence-Based Mindfulness
Getting personal with AI doctors
One of the common reasons that people reject AI doctors is the “lack of a human touch”. However, human and AI doctors may be meeting in the middle nowadays, as humans are pressed to see more patients in less time, and AI is trained to be more personal—not just a friendlier affect, but also, such things as remembering the patient’s previous encounters (again, something with which overworked human doctors sometimes struggle). This makes a big difference to patient satisfaction:
Read in full: Personalization key to patient satisfaction with AI doctors
Related: AI: The Doctor That Never Tires?
Combination brain therapy against cognitive decline
This study found that out of various combinations trialled, the best intervention against cognitive decline was a combination of 1) cognitive remediation (therapeutic interventions designed to improve cognitive functioning, like puzzles and logic problems), and 2) transcranial direct current stimulation (tDCS), a form of non-invasive direct brain stimulation, similar to the magnetic or ultrasound methods we mentioned earlier today. Here’s how it worked:
Read in full: Study reveals effective combination therapy to slow cognitive decline in older adults
Related: How To Reduce Your Alzheimer’s Risk
Take care!
Share This Post
-
For Seniors With Hoarding Disorder, a Support Group Helps Confront Stigma and Isolation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A dozen people seated around folding tables clap heartily for a beaming woman: She’s donated two 13-gallon garbage bags full of clothes, including several Christmas sweaters and a couple of pantsuits, to a Presbyterian church.
A closet cleanout might not seem a significant accomplishment. But as the people in this Sunday-night class can attest, getting rid of stuff is agonizing for those with hoarding disorder.
People with the diagnosis accumulate an excessive volume of things such as household goods, craft supplies, even pets. In extreme cases, their homes become so crammed that moving between rooms is possible only via narrow pathways.
These unsafe conditions can also lead to strained relationships.
“I’ve had a few relatives and friends that have condemned me, and it doesn’t help,” said Bernadette, a Pennsylvania woman in her early 70s who has struggled with hoarding since retiring and no longer allows guests in her home.
People who hoard are often stigmatized as lazy or dirty. NPR, Spotlight PA, and KFF Health News agreed to use only the first names of people with hoarding disorder interviewed for this article because they fear personal and professional repercussions if their condition is made public.
As baby boomers age into the group most affected by hoarding disorder, the psychiatric condition is a growing public health concern. Effective treatments are scarce. And because hoarding can require expensive interventions that drain municipal resources, more funding and expertise is needed to support those with the diagnosis before the issue grows into a crisis.
For Bernadette, the 16-week course is helping her turn over a new leaf.
The program doubles as a support group and is provided through Fight the Blight. The Westmoreland County, Pennsylvania, organization started offering the course at a local Masonic temple after founder Matt Williams realized the area lacked hoarding-specific mental health services.
Fight the Blight uses a curriculum based on cognitive behavioral therapy to help participants build awareness of what fuels their hoarding. People learn to be more thoughtful about what they purchase and save, and they create strategies so that decluttering doesn’t become overwhelming.
Perhaps more importantly, attendees say they’ve formed a community knitted together through the shared experience of a psychiatric illness that comes with high rates of social isolation and depression.
“You get friendship,” said Sanford, a classmate of Bernadette’s.
After a lifetime of judgment, these friendships have become an integral part of the changes that might help participants eventually clear out the clutter.
Clutter Catches Up to Baby Boomers
Studies have estimated that hoarding disorder affects around 2.5% of the general population — a higher rate than schizophrenia.
The mental illness was previously considered a subtype of obsessive-compulsive disorder, but in 2013 it was given its own diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, the DSM-5.
The biological and environmental factors that may drive hoarding are not well understood. Symptoms usually appear during the teenage years and tend to be more severe among older adults with the disorder. That’s partly because they have had more time to acquire things, said Kiara Timpano, a University of Miami psychology professor.
“All of a sudden you have to downsize this huge home with all the stuff and so it puts pressures on individuals,” she said. In Bernadette’s case, her clutter includes a collection of VHS tapes, and spices in her kitchen that she said date back to the Clinton administration.
But it’s more than just having decades to stockpile possessions; the urge to accumulate strengthens with age, according to Catherine Ayers, a psychiatry professor at the University of California-San Diego.
Researchers are working to discern why. Ayers and Timpano theorize that age-related cognitive changes — particularly in the frontal lobe, which regulates impulsivity and problem-solving — might exacerbate the disorder.
“It is the only mental health disorder, besides dementia, that increases in prevalence and severity with age,” Ayers said.
As the U.S. population ages, hoarding presents a growing public health concern: Some 1 in 5 U.S. residents are baby boomers, all of whom will be 65 or older by 2030.
This population shift will require the federal government to address hoarding disorder, among other age-related issues that it has not previously prioritized, according to a July report by the Democratic staff of the U.S. Senate Special Committee on Aging, chaired then by former Sen. Bob Casey (D-Pa.).
Health Hazards of Hoarding
Clutter creates physical risks. A cramped and disorderly home is especially dangerous for older adults because the risk of falling and breaking a bone increases with age. And having too many things in one space can be a fire hazard.
Last year, the National Fallen Firefighters Foundation wrote to the Senate committee’s leadership that “hoarding conditions are among the most dangerous conditions the fire service can encounter.” The group also said that cluttered homes delay emergency care and increase the likelihood of a first responder being injured on a call.
The Bucks County Board of Commissioners in Pennsylvania told Casey that hoarding-related mold and insects can spread to adjacent households, endangering the health of neighbors.
Due to these safety concerns, it might be tempting for a family member or public health agency to quickly empty someone’s home in one fell swoop.
That can backfire, Timpano said, as it fails to address people’s underlying issues and can be traumatic.
“It can really disrupt the trust and make it even less likely that the individual is willing to seek help in the future,” she said.
It’s more effective, Timpano said, to help people build internal motivation to change and help them identify goals to manage their hoarding.
For example, at the Fight the Blight class, a woman named Diane told the group she wanted a cleaner home so she could invite people over and not feel embarrassed.
Sanford said he is learning to keep his documents and record collection more organized.
Bernadette wants to declutter her bedroom so she can start sleeping in it again. Also, she’s glad she cleared enough space on the first floor for her cat to play.
“Because now he’s got all this room,” she said, “he goes after his tail like a crazy person.”
Ultimately, the home of someone with hoarding disorder might always be a bit cluttered, and that’s OK. The goal of treatment is to make the space healthy and safe, Timpano said, not to earn Marie Kondo’s approval.
Lack of Treatment Leaves Few Options
A 2020 study found that hoarding correlates with homelessness, and those with the disorder are more likely to be evicted.
Housing advocates argue that under the Fair Housing Act, tenants with the diagnosis are entitled to reasonable accommodation. This might include allowing someone time to declutter a home and seek therapy before forcing them to leave their home.
But as outlined in the Senate aging committee’s report, a lack of resources limits efforts to carry out these accommodations.
Hoarding is difficult to treat. In a 2018 study led by Ayers, the UCSD psychiatrist, researchers found that people coping with hoarding need to be highly motivated and often require substantial support to remain engaged with their therapy.
The challenge of sticking with a treatment plan is exacerbated by a shortage of clinicians with necessary expertise, said Janet Spinelli, the co-chair of Rhode Island’s hoarding task force.
Could Changes to Federal Policy Help?
Casey, the former Pennsylvania senator, advocated for more education and technical assistance for hoarding disorder.
In September, he called for the Substance Abuse and Mental Health Services Administration to develop training, assistance, and guidance for communities and clinicians. He also said the Centers for Medicare & Medicaid Services should explore ways to cover evidence-based treatments and services for hoarding.
This might include increased Medicare funding for mobile crisis services to go to people’s homes, which is one way to connect someone to therapy, Spinelli said.
Another strategy would involve allowing Medicaid and Medicare to reimburse community health workers who assist patients with light cleaning and organizing; research has found that many who hoard struggle with categorization tasks.
Williams, of Fight the Blight, agrees that in addition to more mental health support, taxpayer-funded services are needed to help people address their clutter.
When someone in the group reaches a point of wanting to declutter their home, Fight the Blight helps them start the process of cleaning, removing, and organizing.
The service is free to those earning less than 150% of the federal poverty level. People making above that threshold can pay for assistance on a sliding scale; the cost varies also depending on the size of a property and severity of the hoarding.
Also, Spinelli thinks Medicaid and Medicare should fund more peer-support specialists for hoarding disorder. These mental health workers draw on their own life experiences to help people with similar diagnoses. For example, peer counselors could lead classes like Fight the Blight’s.
Bernadette and Sanford say courses like the one they enrolled in should be available all over the U.S.
To those just starting to address their own hoarding, Sanford advises patience and persistence.
“Even if it’s a little job here, a little job there,” he said, “that all adds up.”
This article is from a partnership that includes Spotlight PA, NPR, and KFF Health News.
Spotlight PA is an independent, nonpartisan, and nonprofit newsroom producing investigative and public-service journalism that holds power to account and drives positive change in Pennsylvania. Sign up for its free newsletters.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
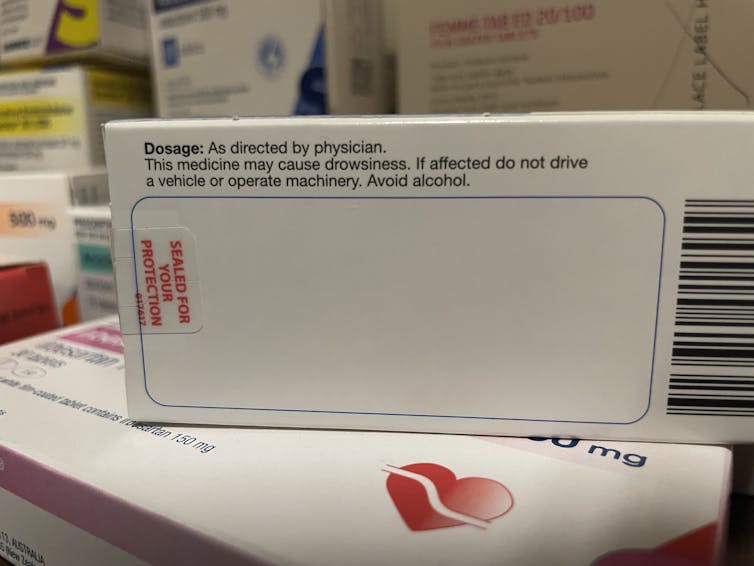
Why it’s a bad idea to mix alcohol with some medications
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anyone who has drunk alcohol will be familiar with how easily it can lower your social inhibitions and let you do things you wouldn’t normally do.
But you may not be aware that mixing certain medicines with alcohol can increase the effects and put you at risk.
When you mix alcohol with medicines, whether prescription or over-the-counter, the medicines can increase the effects of the alcohol or the alcohol can increase the side-effects of the drug. Sometimes it can also result in all new side-effects.
How alcohol and medicines interact
The chemicals in your brain maintain a delicate balance between excitation and inhibition. Too much excitation can lead to convulsions. Too much inhibition and you will experience effects like sedation and depression.
Alcohol works by increasing the amount of inhibition in the brain. You might recognise this as a sense of relaxation and a lowering of social inhibitions when you’ve had a couple of alcoholic drinks.
With even more alcohol, you will notice you can’t coordinate your muscles as well, you might slur your speech, become dizzy, forget things that have happened, and even fall asleep.
Alcohol can affect the way a medicine works.
Jonathan Kemper/UnsplashMedications can interact with alcohol to produce different or increased effects. Alcohol can interfere with the way a medicine works in the body, or it can interfere with the way a medicine is absorbed from the stomach. If your medicine has similar side-effects as being drunk, those effects can be compounded.
Not all the side-effects need to be alcohol-like. Mixing alcohol with the ADHD medicine ritalin, for example, can increase the drug’s effect on the heart, increasing your heart rate and the risk of a heart attack.
Combining alcohol with ibuprofen can lead to a higher risk of stomach upsets and stomach bleeds.
Alcohol can increase the break-down of certain medicines, such as opioids, cannabis, seizures, and even ritalin. This can make the medicine less effective. Alcohol can also alter the pathway of how a medicine is broken down, potentially creating toxic chemicals that can cause serious liver complications. This is a particular problem with paracetamol.
At its worst, the consequences of mixing alcohol and medicines can be fatal. Combining a medicine that acts on the brain with alcohol may make driving a car or operating heavy machinery difficult and lead to a serious accident.
Who is at most risk?
The effects of mixing alcohol and medicine are not the same for everyone. Those most at risk of an interaction are older people, women and people with a smaller body size.
Older people do not break down medicines as quickly as younger people, and are often on more than one medication.
Older people also are more sensitive to the effects of medications acting on the brain and will experience more side-effects, such as dizziness and falls.
Smaller and older people are often more affected.
Alfonso Scarpa/UnsplashWomen and people with smaller body size tend to have a higher blood alcohol concentration when they consume the same amount of alcohol as someone larger. This is because there is less water in their bodies that can mix with the alcohol.
What drugs can’t you mix with alcohol?
You’ll know if you can’t take alcohol because there will be a prominent warning on the box. Your pharmacist should also counsel you on your medicine when you pick up your script.
The most common alcohol-interacting prescription medicines are benzodiazepines (for anxiety, insomnia, or seizures), opioids for pain, antidepressants, antipsychotics, and some antibiotics, like metronidazole and tinidazole.
Medicines will carry a warning if you shouldn’t take them with alcohol.
Nial WheateIt’s not just prescription medicines that shouldn’t be mixed with alcohol. Some over-the-counter medicines that you shouldn’t combine with alcohol include medicines for sleeping, travel sickness, cold and flu, allergy, and pain.
Next time you pick up a medicine from your pharmacist or buy one from the local supermarket, check the packaging and ask for advice about whether you can consume alcohol while taking it.
If you do want to drink alcohol while being on medication, discuss it with your doctor or pharmacist first.
Nial Wheate, Associate Professor of the School of Pharmacy, University of Sydney; Jasmine Lee, Pharmacist and PhD Candidate, University of Sydney; Kellie Charles, Associate Professor in Pharmacology, University of Sydney, and Tina Hinton, Associate Professor of Pharmacology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fasting, eating earlier in the day or eating fewer meals – what works best for weight loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, one in eight people are living with obesity. This is an issue because excess fat increases the risk of type 2 diabetes, heart disease and certain cancers.
Modifying your diet is important for managing obesity and preventing weight gain. This might include reducing your calorie intake, changing your eating patterns and prioritising healthy food.
But is one formula for weight loss more likely to result in success than another? Our new research compared three weight-loss methods, to see if one delivered more weight loss than the others:
- altering calorie distribution – eating more calories earlier rather than later in the day
- eating fewer meals
- intermittent fasting.
We analysed data from 29 clinical trials involving almost 2,500 people.
We found that over 12 weeks or more, the three methods resulted in similar weight loss: 1.4–1.8kg.
So if you do want to lose weight, choose a method that works best for you and your lifestyle.
chalermphon_tiam/Shutterstock Eating earlier in the day
When our metabolism isn’t functioning properly, our body can’t respond to the hormone insulin properly. This can lead to weight gain, fatigue and can increase the risk of a number of chronic diseases such as diabetes.
Eating later in the day – with a heavy dinner and late-night snacking – seems to lead to worse metabolic function. This means the body becomes less efficient at converting food into energy, managing blood sugar and regulating fat storage.
In contrast, consuming calories earlier in the day appears to improve metabolic function.
However, this might not be the case for everyone. Some people naturally have an evening “chronotype”, meaning they wake up and stay up later.
People with this chronotype appear to have less success losing weight, no matter the method. This is due to a combination of factors including genes, an increased likelihood to have a poorer diet overall and higher levels of hunger hormones.
Eating fewer meals
Skipping breakfast is common, but does it hinder weight loss? Or is a larger breakfast and smaller dinner ideal?
While frequent meals may reduce disease risk, recent studies suggest that compared to eating one to two meals a day, eating six times a day might increase weight loss success.
However, this doesn’t reflect the broader research, which tends to show consuming fewer meals can lead to greater weight loss. Our research suggests three meals a day is better than six. The easiest way to do this is by cutting out snacks and keeping breakfast, lunch and dinner.
Most studies compare three versus six meals, with limited evidence on whether two meals is better than three.
However, front-loading your calories (consuming most of your calories between breakfast and lunch) appears to be better for weight loss and may also help reduce hunger across the day. But more studies with a longer duration are needed.
Fasting, or time-restricted eating
Many of us eat over a period of more than 14 hours a day.
Eating late at night can throw off your body’s natural rhythm and alter how your organs function. Over time, this can increase your risk of type 2 diabetes and other chronic diseases, particularly among shift workers.
Time-restricted eating, a form of intermittent fasting, means eating all your calories within a six- to ten-hour window during the day when you’re most active. It’s not about changing what or how much you eat, but when you eat it.
Some people limit their calories to a six hour window, while others opt for ten hours. Shutterstock/NIKS ADS Animal studies suggest time-restricted eating can lead to weight loss and improved metabolism. But the evidence in humans is still limited, especially about the long-term benefits.
It’s also unclear if the benefits of time-restricted eating are due to the timing itself or because people are eating less overall. When we looked at studies where participants ate freely (with no intentional calorie limits) but followed an eight-hour daily eating window, they naturally consumed about 200 fewer calories per day.
What will work for you?
In the past, clinicians have thought about weight loss and avoiding weight gain as a simile equation of calories in and out. But factors such as how we distribute our calories across the day, how often we eat and whether we eat late at night may also impact our metabolism, weight and health.
There are no easy ways to lose weight. So choose a method, or combination of methods, that suits you best. You might consider
- aiming to eat in an eight-hour window
- consuming your calories earlier, by focusing on breakfast and lunch
- opting for three meals a day, instead of six.
The average adult gains 0.4 to 0.7 kg per year. Improving the quality of your diet is important to prevent this weight gain and the strategies above might also help.
Finally, there’s still a lot we don’t know about these eating patterns. Many existing studies are short-term, with small sample sizes and varied methods, making it hard to make direct comparisons.
More research is underway, including well-controlled trials with larger samples, diverse populations and consistent methods. So hopefully future research will help us better understand how altering our eating patterns can result in better health.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University and Loai Albarqouni, Assistant Professor | NHMRC Emerging Leadership Fellow, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We looked at genetic clues to depression in more than 14,000 people. What we found may surprise you
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The core experiences of depression – changes in energy, activity, thinking and mood – have been described for more than 10,000 years. The word “depression” has been used for about 350 years.
Given this long history, it may surprise you that experts don’t agree about what depression is, how to define it or what causes it.
But many experts do agree that depression is not one thing. It’s a large family of illnesses with different causes and mechanisms. This makes choosing the best treatment for each person challenging.
Reactive vs endogenous depression
One strategy is to search for sub-types of depression and see whether they might do better with different kinds of treatments. One example is contrasting “reactive” depression with “endogenous” depression.
Reactive depression (also thought of as social or psychological depression) is presented as being triggered by exposure to stressful life events. These might be being assaulted or losing a loved one – an understandable reaction to an outside trigger.
Endogenous depression (also thought of as biological or genetic depression) is proposed to be caused by something inside, such as genes or brain chemistry.
Many people working clinically in mental health accept this sub-typing. You might have read about this online.
But we think this approach is way too simple.
While stressful life events and genes may, individually, contribute to causing depression, they also interact to increase the risk of someone developing depression. And evidence shows that there is a genetic component to being exposed to stressors. Some genes affect things such as personality. Some affect how we interact with our environments.
What we did and what we found
Our team set out to look at the role of genes and stressors to see if classifying depression as reactive or endogenous was valid.
In the Australian Genetics of Depression Study, people with depression answered surveys about exposure to stressful life events. We analysed DNA from their saliva samples to calculate their genetic risk for mental disorders.
Our question was simple. Does genetic risk for depression, bipolar disorder, schizophrenia, ADHD, anxiety and neuroticism (a personality trait) influence people’s reported exposure to stressful life events?
We looked at the genetic risk of mental illness to see how that was linked to stressful life events, such as childhood abuse and neglect. Kamira/Shutterstock You may be wondering why we bothered calculating the genetic risk for mental disorders in people who already have depression. Every person has genetic variants linked to mental disorders. Some people have more, some less. Even people who already have depression might have a low genetic risk for it. These people may have developed their particular depression from some other constellation of causes.
We looked at the genetic risk of conditions other than depression for a couple of reasons. First, genetic variants linked to depression overlap with those linked to other mental disorders. Second, two people with depression may have completely different genetic variants. So we wanted to cast a wide net to look at a wider spectrum of genetic variants linked to mental disorders.
If reactive and endogenous depression sub-types are valid, we’d expect people with a lower genetic component to their depression (the reactive group) would report more stressful life events. And we’d expect those with a higher genetic component (the endogenous group) would report fewer stressful life events.
But after studying more than 14,000 people with depression we found the opposite.
We found people at higher genetic risk for depression, anxiety, ADHD or schizophrenia say they’ve been exposed to more stressors.
Assault with a weapon, sexual assault, accidents, legal and financial troubles, and childhood abuse and neglect, were all more common in people with a higher genetic risk of depression, anxiety, ADHD or schizophrenia.
These associations were not strongly influenced by people’s age, sex or relationships with family. We didn’t look at other factors that may influence these associations, such as socioeconomic status. We also relied on people’s memory of past events, which may not be accurate.
How do genes play a role?
Genetic risk for mental disorders changes people’s sensitivity to the environment.
Imagine two people, one with a high genetic risk for depression, one with a low risk. They both lose their jobs. The genetically vulnerable person experiences the job loss as a threat to their self-worth and social status. There is a sense of shame and despair. They can’t bring themselves to look for another job for fear of losing it too. For the other, the job loss feels less about them and more about the company. These two people internalise the event differently and remember it differently.
Genetic risk for mental disorders also might make it more likely people find themselves in environments where bad things happen. For example, a higher genetic risk for depression might affect self-worth, making people more likely to get into dysfunctional relationships which then go badly.
If two people lose their jobs, one with a high genetic risk of depression the other at low risk, both will experience and remember the event differently. Inside Creative House/Shutterstock What does our study mean for depression?
First, it confirms genes and environments are not independent. Genes influence the environments we end up in, and what then happens. Genes also influence how we react to those events.
Second, our study doesn’t support a distinction between reactive and endogenous depression. Genes and environments have a complex interplay. Most cases of depression are a mix of genetics, biology and stressors.
Third, people with depression who appear to have a stronger genetic component to their depression report their lives are punctuated by more serious stressors.
So clinically, people with higher genetic vulnerability might benefit from learning specific techniques to manage their stress. This might help some people reduce their chance of developing depression in the first place. It might also help some people with depression reduce their ongoing exposure to stressors.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jacob Crouse, Research Fellow in Youth Mental Health, Brain and Mind Centre, University of Sydney and Ian Hickie, Co-Director, Health and Policy, Brain and Mind Centre, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: